G6PD Deficiency
Introduction
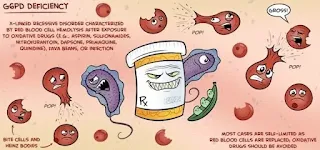
G6PD deficiency (Glucose-6-phosphate dehydrogenase deficiency) is an inherited condition in which patients are excessively susceptible to the development of haemolytic anaemia.
- Affected people lack the ability to tolerate biochemical oxidative stress.
- Almost all patients are completely asymptomatic, but infections, drugs or ingesting broad beans can precipitate haemolysis.
- Newborns may have prolonged and/or severe neonatal hyperbilirubinemia.
Aetiology
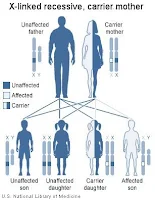
Since G6PD deficiency is an X-linked disorder, males are more likely to be affected, and heterozygous females are typically unaffected carriers, but females who are homozygous, compound heterozygous or heterozygous with skewed lyonization can have significant haemolysis.
NOTE: Pregnant and nursing women who are heterozygous G6PD deficiency should avoid drugs known to be unsafe because some of these drugs gain access to the foetal circulation and to breast milk.
WHO Classification
World Health Organization classifies G6PD deficiency according to the magnitude of the enzyme deficiency and the severity of haemolysis.
- Class I: Severely deficient, associated with chronic non-spherocytic haemolytic anaemia
- Class II: Severely deficient (1%-10% residual activity), associated with acute haemolytic anaemia
- Class III: Moderately deficient (10%-60% residual activity)
- Class IV: Normal activity (60%-150%)
- Class V: Increased activity (>150%).
Only class I, II and II are of clinical significance.
Management
The cornerstone of management of G6PD deficiency is the avoidance of oxidative stress to red blood cells, once the diagnosis is made.
- However, there may be instances in which an oxidant drug is absolutely required, or cases in which oxidative stress comes from an infection or other acute medical condition that cannot be avoided.
- In these settings, management depends on the severity of haemolysis and anaemia and the patient's age and comorbidities.
Patients diagnosed with G6PD deficiency should seek medical attention whenever any of the following symptoms develop:
- Jaundice (yellow skin and eyes)
- Dark coloured urine
- Anaemia (pale skin and lethargy).
Drugs to Avoid
Two important reminders that I would like to highlight here:
- Drug manufacturers do not routinely carry out testing to identify the potential risk of their drug to G6PD-deficient patients. Do not assume with new drugs that if there is no warning in the SPC, the drug is safe.
- Susceptibility to the haemolytic risk from drugs varies; a drug found to be safe in some G6PD-deficient patients may not be equally safe in others.
Drugs with definite risk of haemolytic anaemia in most G6PD-deficient patients (avoid)
- Dapsone and other sulphones
- Methylthioninium chloride (methylene blue)
- Nitrofurantoin
- Primaquine
- Quinolones
- Rasburicase
- Sulfonamides (including co-trimoxazole)
Drugs with possible risk of haemolytic anaemia in some G6PD-deficient patients (caution)*
- Aminosalicylic acid
- Ascorbic acid
- Aspirin (doses >1g/day)
- Chloramphenicol
- Chloroquine†
- Hydroxychloroquine
- Isoniazid
- Levodopa
- Menadione (water-soluble vitamin K derivatives)
- Probenecid
- Pyrimethamine
- Quinidine†
- Quinine†
- Streptomycin
- Sulfonylureas * Use with caution; low doses probably safe
† Acceptable to treat acute malaria at usual doses.
Comments
Post a Comment