Chronic Obstructive Pulmonary Disease
Introduction
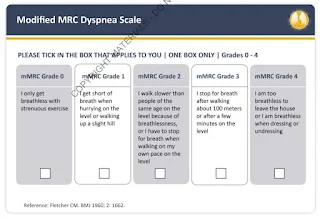
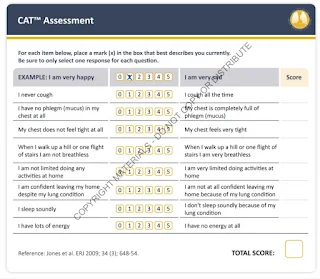
- The most common respiratory symptoms include dyspnoea, cough and/or sputum production.
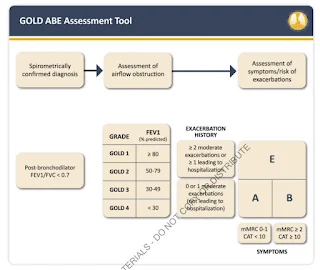
Forced spirometry that demonstrates the presence of a post-bronchodilator FEV1/FVC <0.7 is mandatory to establish the diagnosis of COPD.
GOLD 2023
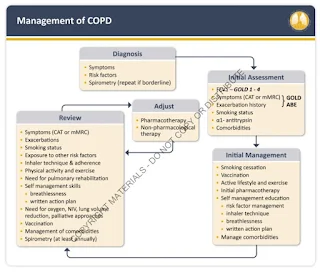
Apart from smoking cessation and vaccination [e.g. COVID-19, pneumococcal and influenza vaccines (and zoster vaccine to protect against shingles for people with COPD over 50 years)], pharmacological therapy for COPD is used:
- to reduce symptoms
- to reduce the frequency and severity of exacerbations
- improve exercise tolerance and health status
Inhaled bronchodilators in COPD are central to symptom management and commonly given on a regular basis to prevent or reduce symptoms.
- Regular and as-needed use of SABA or SAMA improves FEV1 and symptoms.
- Combinations of SABA and SAMA are superior compared to either medication alone in improving FEV1 and symptoms.
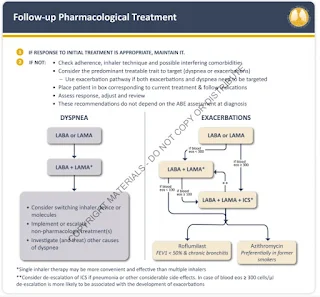
- LABAs and LAMAs significantly improve lung function, dyspnoea, health status and reduce exacerbation rates.
- LAMAs have a greater effect on exacerbation reduction compared with LABAs and decrease hospitalizations.
- Combination treatment with a LABA and LAMA increases FEV1, reduce symptoms and reduce exacerbations compared to monotherapy.
- Tiotropium improves the effectiveness of pulmonary rehabilitation in increasing exercise performance.
- Theophylline exerts a small bronchodilator effect in stable COPD and that is associated with modest symptomatic benefits.
- An ICS combined with a LABA is more effective than the individual components in improving lung function and health status and reducing exacerbations in patients with exacerbations and moderate to very severe COPD. Nonetheless, use of LABA+ICS in COPD is discouraged.
- Regular treatment with ICS increases the risk of pneumonia especially in those with severe disease.
- Triple inhaled therapy with LAMA+LABA+ICS improves lung function, symptoms and health status and reduces exacerbations compared to LABA+ICS, LABA+LAMA, or LAMA monotherapy.
- Long-term use of oral glucocorticoids has numerous side effects with no evidence of benefits.
- Regular treatment with mucolytics such as erdosteine, carbocisteine and N-acetylcysteine reduces the risk of exacerbation in select populations.
Berodual-N in COPD
Few weeks ago, my friend asked me, although Berodual-N MDI consists of fenoterol (SABA) and Ipratropium (SAMA), why are we still commonly using Berodual-N in chronic COPD management?
If you read GOLD 2023,
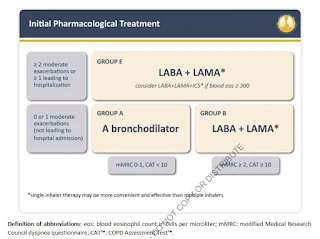
- All Group A patients should be offered bronchodilator treatment (either a short- or a long-acting bronchodilator). If available and affordable, a long-acting bronchodilator is the preferred choice except in patients with very occasional breathlessness.
- In Group B patients, treatment should be initiated with a LABA+LAMA combination. If a LABA+LAMA combination is not considered appropriate, there is no evidence to recommend one class of long-acting bronchodilators over another (LABA or LAMA) for initial relief of symptoms.
- Any exacerbation that lead to hospitalization will put the patient in Group E, where LABA+LAMA is the preferred choice, provided there are no issues regarding availability, cost and side-effects.
In summary, the prevalent use of Berodual-N could be due to resource-limited settings.
NOTE: Ipratropium is not usually used for symptom relief in COPD. It is contraindicated in patients taking a long-acting muscarinic antagonist (LAMA), is more expensive than a SABA and may increase the risk of cardiovascular events.
Comments
Post a Comment