Smoking Cessation
Introduction
Smoking represents the single greatest cause of preventable illness and premature death worldwide.
- The risks of most harms from tobacco smoking correlate with cumulative exposure.
Hundreds of compounds have been identified in tobacco smoke; however, only 3 compounds are of real clinical importance:
- Tar-based products, which have carcinogenic properties.
- Carbon monoxide, which reduces the oxygen-carrying capacity of the red blood cells.
- Nicotine, which produces dependence by activation of dopaminergic systems.
Stopping Smoking
Health benefits from smoking cessation are well documented and quitting smoking before 35 years of age avoids almost all excess risk for developing smoking-related diseases.
Stopping smoking often causes unpleasant withdrawal effects (craving, anxiety, irritability, restlessness, poor concentration, light-headedness, hunger). These symptoms may begin within a few hours of the last cigarette, peak after a few days and rarely last >1 month.
NOTE: Chemicals in tobacco smoke increase the metabolism of certain drugs metabolized by CYP1A2, e.g. clozapine, theophylline, and it may be necessary to reduce their dosage soon after smoking is stopped.
Non-drug Treatment
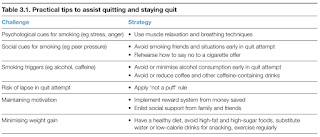
Provide counselling and discuss behavioural techniques to aid and encourage smoking cessation.
Drug Treatment
Pharmacotherapy should be recommended to all people who smoke with nicotine dependence. However, an individual's choice to attempt to quit without assistance should be respected and supported.
Nicotine replacement therapy
- NRT increases rates of quitting smoking by 50 to 60%.
- All forms of NRT (e.g. gum, lozenges, patches, nasal spray, inhalator) are effective and there are insufficient data to suggest that one form is superior to another.
- Choice depends upon the smoker's preference.
- Patches should be applied to non-hairy skin on the hip, chest or upper arm. The next patch should be placed on a different site to avoid skin irritation. A 16-hour patch will be suitable for most patients (since sleep disturbances may be experienced with the 24-hour patches); however, if a patient requires a cigarette within the first 20-30 minutes after waking, then a 24-hour patch should be given.
- The gum should be chewed slowly until the taste becomes strong, it should then be rested between the cheek and gum until the taste fades. The gum can then be re-chewed. Each piece of gum lasts approximately 30 minutes.
- Controlled trials have shown that a combination of a transdermal nicotine patch and a short-acting form of NRT (e.g. patch plus gum) can be more effective than using a single form of NRT.
- Continue treatment for up to 12 weeks (6-8 weeks for most people), including the taper period. Treatment for longer periods may be useful in some cases.
Varenicline (Champix)
- Partial agonist at nicotine receptors; It reduces withdrawal symptoms and the pleasurable effects of smoking.
- Varenicline more than doubles the number of people quitting compared with placebo and appears to have similar efficacy to combination NRT (nicotine patches with a faster-acting NRT) and to be more effective than bupropion.
- Varenicline is started while the person is still smoking, and a quit date is set for the second week of therapy but there can be flexibility around the timing of beginning treatment. The usual dose is
- Varenicline 0.5 mg orally, daily for 3 days, then 0.5 mg twice daily for 4 days, then 1 mg twice daily for the remainder of a 12-week course.
- Nausea is the most common adverse effect (30%) and can be reduced by taking varenicline with food.
- There is concern about neuropsychiatric adverse effects and people taking varenicline should be monitored for unusual mood changes, depression, behaviour disturbance and suicidal thoughts.
Bupropion
- Bupropion is started while the person is still smoking, and a quit date is set for the second week of therapy but many people stop smoking sooner. It takes about a week for bupropion plasma steady-state concentration to be reached and doses higher than bupropion 300 mg daily are not recommended because of the risk of dose-dependent seizures. The usual dose is:
- Bupropion 150 mg orally, once daily for 3 days, then 150 mg twice daily for the remainder of a 9-week course.
- It causes insomnia in >40% of patients (20% with placebo); its potential to cause seizure limits its use.
E-Cigarettes (Nicotine Vaping)
When other measures are not successful or suitable in the management of nicotine dependence, nicotine vaping products are often used as second-line therapy as harm minimisation approach.
- A majority of e-cigarette users perceive them to be a tool to quit or reduce their smoking.
- Nonetheless, advise patients to avoid concurrent use of nicotine vaping products and tobacco to maximise benefit and minimize harm.
E-cigarettes deliver nicotine without the toxins found in tobacco smoke.
- Evidence suggests that e-cigarettes are substantially less harmful to health than tobacco smoking, but long-term effects are still largely unknown.
E-cigarette, or vaping, product use associated lung injury [EVALI]) is a rare, but potentially fatal respiratory illness in which individuals develop pneumonia associated with lipid-laden macrophages in the lungs.
- EVALI may occur with nicotine-only vaping liquid but more commonly occurs with vaping liquids containing tetrahydrocannabinol (THC), vitamin E acetate and oil-containing additives.
NOTE: While vaping is considered less harmful than traditional cigarettes, it is important to note that it is not without risk. Hence, vaping is not recommended for those who have never smoked before.
Referral
Behavioural change is complex. Relapse is a normal part of the quitting process and occurs on average three to four times.
- If a smoker has made repeated attempts to stop and has failed, experienced severe withdrawal or has requested more intensive help, then referral to a specialist smoking cessation service should be considered.
External Links
- Nicotine replacement therapy versus control for smoking cessation, 2018
- Characteristics of Hospitalized and Nonhospitalized Patients in a Nationwide Outbreak of E-cigarette, or Vaping, Product Use-Associated Lung Injury, 2019
- RACGP Supporting Smoking Cessation, 2019
- Electronic cigarettes for smoking cessation, 2022
- NHMS Survey: Among Malaysian Teens, Smoking Rate Falls But Vaping Prevalence Rises To 15%, 2023
- Therapeutic vapes for smoking cessation and nicotine dependence, 2024


Comments
Post a Comment