Depression
Introduction
People with major depression typically have a low mood, loss of interest and enjoyment in activities, and other psychological and somatic symptoms.
- Somatic symptoms
- Changes to weight
- Psychomotor disturbance (agitation or retardation)
- Fatigue and sleep disturbance (either insomnia or hypersomnia)
- Psychological symptoms
- Diminished concentration
- Low self-esteem
- Excessive guilt
- Feelings of hopelessness and helplessness
- Suicidal thoughts or ambivalence about living
Management
Psychoeducation should be accompanied by support to help the patient modify their lifestyle, if necessary.
- Lifestyle modification can include improving sleep hygiene, undertaking adequate physical activity (exercise), consuming a healthy diet, minimising alcohol consumption, reducing stress, and reviewing daily routines and social support.
Using a shared decision-making approach when discussing further treatment options (psychological therapies, antidepressants or both) with patients.
- Psychological therapies (e.g. cognitive behavioural therapy and interpersonal therapy) are preferred in mild major depression.
- Combination is more effective than either intervention alone.
Electroconvulsive therapy (ECT) may be considered for some forms of severe depression (e.g. melancholic depression)
- The usual cycle is 2 or 3 treatments per week.
- Temporary memory loss is common, and medications that affect seizure threshold must be withdrawn before treatment.
Antidepressant Therapy
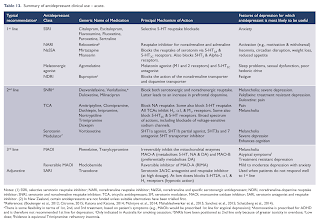
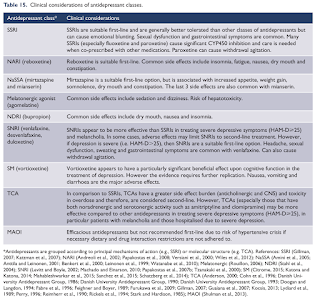
Effectiveness of antidepressants appears generally comparable between drug classes and within classes, with response rates in clinical trials ranging 50-70%.
Initial selection of antidepressant medication for treatment of major depressive disorder should be based on several factors, including anticipated adverse effects, safety or tolerability, and pharmacological properties (as well as prior medication response if a previous treatment episode has occurred).
- Remember, patients frequently discontinue antidepressant medication due to common adverse events.
Selective serotonin reuptake inhibitors (SSRIs) or serotonin norepinephrine reuptake inhibitors (SNRIs) generally considered first-line options for depression because of fewer adverse effects, fewer serious drug interactions, and less lethality in overdose compared to tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs).
Physical symptoms (energy levels, sleep disturbances) improve before affective symptoms. Symptoms can respond as early as 2 weeks.
- In general, it takes 4-6 weeks to see the full effect of antidepressants, given the correct drug, dose, and adherence, but it may take as long as 8 weeks to see a response.
- Remission may take up to 12 weeks.
Approximately a third of patients do not respond to the first antidepressant that is prescribed.
- Options in this group include gradual dose escalation, switching to a different drug (either from the same class or from a different class) and a number of augmentation strategies.
A reasonable amount of evidence suggests that they should be taken for 6-9 months after recovery from a single episode (presumably to cover the duration of an untreated episode).
- In those patients who have had multiple episodes, there is evidence of benefit from maintenance treatment for at least 2 years, but no upper duration of treatment has been identified.
Switching Antidepressants
The most conservative strategy, with the lowest risk of drug interactions, is to gradually taper the dose of the first antidepressant to minimise withdrawal symptoms then start a washout period equivalent to five half-lives of the drug. The second antidepressant is then introduced according to the starting dose recommendations.
- Discontinuation symptoms may occur.
NOTE: Patients using fluoxetine should wait 4-7 days before starting other SSRI due to long half-life.
Cross-titration (gradually reducing dose of old drug while increasing dose of new drug) is recommended when switching to antidepressant with different mechanism (unless new drug is monoamine oxidase inhibitor [MAOI] which should not be taken with SSRIs).
Drug interactions with MAOIs are considerable and include over-the-counter decongestants, antidepressants, stimulants, and antihypertensives.
- When changing a patient from another antidepressant to an MAOI, it is prudent to wait 2 weeks after the antidepressant is discontinued before initiating the MAOI (except for fluoxetine, in which case the waiting period should be 5-6 weeks) to avoid serotonin toxicity.
- When a patient is changed from an MAOI to another antidepressant, a 2-week washout period is usually adequate.
NOTE: Click here to learn more on serotonin syndrome.
Antidepressant Discontinuation Syndrome
To discontinue antidepressants, supervised tapering of medication (including SSRIs, SNRIs, TCA and mirtazapine) should occur over 6-8 weeks; if withdrawal symptoms (also called discontinuation syndrome) occur, consider restarting at original dose and taper at slower pace.
- Agomelatine and vortioxetine has a very low risk of discontinuation symptoms and hence, abrupt withdrawal is possible.
The mnemonic FINISH summarizes the symptoms of antidepressant discontinuation syndrome:
- Flu-like symptoms (lethargy, fatigue, headache, achiness, sweating),
- Insomnia (with vivid dreams or nightmares),
- Nausea (sometimes vomiting),
- Imbalance (dizziness, vertigo, light-headedness),
- Sensory disturbances (“burning,” “tingling,” “electric-like” or “shock-like” sensations) and
- Hyperarousal (anxiety, irritability, agitation, aggression, mania, jerkiness).
Diet and Mental Health
There is increasing evidence of a relationship between diet and mental health.
- Adherence to a Mediterranean diet (high intake of vegetables, fruits, nuts, cereals, legumes and fish) has been associated with a decreased risk of depression.
- Additionally, diets with high levels of processed foods have been found to contribute to depressive symptoms.
Complementary Medicines
Complementary medicines are commonly used by patients with major depression but their safety, quality and efficacy are not well established. In some instances, their use can lead to significant drug interactions or adverse effects.
St John's wort and omega-3 fatty acids have the most evidence of efficacy for major depression.
- Studies have shown that extracts of St John's wort are effective for the treatment of mild to moderate major depression in adults.
- Omega-3 fatty acids may be beneficial in the treatment of major depression but there is not adequate evidence to support their routine use.
External Links
- eTG Complete - Major Depression
- DynaMed - Antidepressant Medication Overview
- Beyond Blue Resource Library
- FINISH: remembering the discontinuation syndrome. Flu-like symptoms, Insomnia, Nausea, Imbalance, Sensory disturbances, and Hyperarousal (anxiety/agitation), 1998
- The Rise of All-Purpose Antidepressants, 2014
- Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders, 2015
- Switching and Stopping Antidepressants, 2016
- Drug-Induced Serotonin Syndrome, 2017
- Diet quality and depression risk: A systematic review and dose-response meta-analysis of prospective studies, 2018
- Improved efficacy with targeted pharmacogenetic-guided treatment of patients with depression and anxiety: A randomized clinical trial demonstrating clinical utility, 2018
- Malaysia Management of Major Depressive Disorder, 2019
- Efficacy of omega-3 PUFAs in depression: A meta-analysis, 2019
- Esketamine Nasal Spray for Treatment-Resistant Depression, 2020


Comments
Post a Comment