Insomnia
Introduction
Insomnia can be broken down into difficulty in getting to sleep, difficulty staying sleep, early waking or feeling unsatisfied by sleep, despite adequate time and opportunity to sleep. Often a mixture of these can occur.
These are associated with complaints of impaired daytime functioning, such as poor concentration and memory, mood disturbances and daytime tiredness.
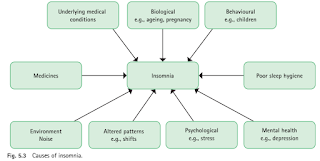
Etiology
Insomnia may be caused by any factor that increases activity in arousal systems or decreases activity in sleep systems.
NOTE: In older people, the total duration of sleep is shorter and there is less deep (stage 4) sleep. Moreover, older people may nap during the day and this reduces their sleep need at night even further.
Referral to Doctor
Cases of chronic insomnia (>4 weeks) are best referred to the doctor, as there is usually an underlying cause.
NOTE: People with chronic insomnia are at higher risk of medical conditions (e.g. cardiovascular disease, diabetes, psychiatric disorders (e.g. depression, anxiety) and premature death.
Sleep Hygiene
Many cases of short-term insomnia should be managed initially by nonpharmacological measures. If these fail to rectify the problem, short-term use of sedating antihistamines (e.g. promethazine) may be tried.
- Maintain a routine, with a regular bedtime and awakening time.
- No sleeping in to catch up on sleep.
- Avoid daytime naps (if necessary, limit to an afternoon "powernap" of 15 to 30 minutes).
- No watching TV or using phones, tablets or computers shortly before going to bed. If screens cannot be avoided, blue-light filtering glasses or blue-light screen filters may reduce the effect of blue light.
- Ensure a quiet, cool, dark room for sleep
- Avoid caffeine, nicotine and alcohol within 6 hours of going to bed.
- Avoid exercise within 4 hours of bedtime (although exercise earlier in the day is beneficial).
- Avoid checking the clock through the night; this increases anxiety.
- Try to create a relaxation period before going to bed. Try taking a warm bath 1-2 hours (not immediately) before bedtime or listening to calm music.
- Only use the bedroom for sleep and sexual activity.
- If unable to sleep after 20 minutes, get up and do something relaxing and return to bed when sleepy.
Complementary Therapies
A 2006 systematic review identified 16 studies comparing valerian to placebo and suggests that valerian might improve sleep quality without producing side effects. However, most studies had significant methodological problems, and the valerian doses, preparations and length of treatment varied considerably.
- Valerian should be taken approximately 1 hour prior to bedtime. Continuous nightly use of valerian may be needed for significant effect for some people.
Melatonin is advocated for sleep disturbance, particularly associated with jet lag.
- There is no melatonin supplement registered in Malaysia.
- However, consumption of a tart cherry juice concentrate provides an increase in exogenous melatonin that is beneficial in improving sleep duration and quality in healthy men and women and might be of benefit in managing disturbed sleep.
- Kava supplements may have a small effect on reducing anxiety, but they have been linked to a risk of severe liver injury. For this reason, the use of kava has been banned or restricted in many countries of the world such as Germany, Switzerland, France, Canada, and Great Britain.
External Links
- Melatonin for the prevention and treatment of jet lag, 2002
- Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan, 2004
- The Efficacy and Safety of Exogenous Melatonin for Primary Sleep Disorders, 2005
- Valerian for Sleep: A Systematic Review and Meta-Analysis, 2006
- A systematic review of valerian as a sleep aid: safe but not effective, 2007
- Effect of tart cherry juice (Prunus cerasus) on melatonin levels and enhanced sleep quality, 2012
- Sleep Habits, Insomnia, and Daytime Sleepiness in a Large and Healthy Community-Based Sample of New Zealanders, 2013
- A Comparison of Blue Light and Caffeine Effects on Cognitive Function and Alertness in Humans, 2013
- Herbal medicine for insomnia: A systematic review and meta-analysis, 2015
- National Sleep Foundation's sleep time duration recommendations: methodology and results summary, 2015
- Association of Longitudinal Patterns of Habitual Sleep Duration With Risk of Cardiovascular Events and All-Cause Mortality, 2020
Comments
Post a Comment