Diabetes Mellitus
Introduction
The term diabetes mellitus describes diseases of abnormal carbohydrate metabolism that are characterized by hyperglycemia. It is associated with
- A relative or absolute impairment in insulin secretion, along with
- Varying degrees of peripheral resistance to the action of insulin.
Fasting plasma glucose (FPG), two-hour plasma glucose during a 75 g oral glucose tolerance test (OGTT) or glycated hemoglobin (A1c) may be used for diagnostic testing.
- OGTT is not commonly used (except during pregnancy) owing to its inconvenience.
- Hemoglobin A combines with glucose to form glycosylated hemoglobin. The proportion of hemoglobin in the glycated form (HbA1c) gives an indication of the blood glucose concentration over the preceding three months (the life of a red blood cell).
Morbidity from diabetes is a consequence of both
- Macrovascular disease (atherosclerosis) and
- Microvascular (retinopathy, nephropathy and neuropathy).
NOTE: Gestational diabetes mellitus will be discussed in a separate post.
Type 1 Diabetes Mellitus
Type 1 diabetes is characterized by autoimmune destruction of the pancreatic beta cells, leading to absolute insulin deficiency.
- It usually presents in childhood or early adulthood but can present in any stage of life.
- DKA may be the initial presentation in approximately 25 percent of adults with newly diagnosed type 1 diabetes.
The standard of care for patients with type 1 diabetes is intensive diabetes therapy.
- It includes the coordination of meals/diets and activity with insulin replacement as physiologically as possible, which involves the frequent monitoring of glucose levels and frequent insulin administration to match needs.
The recommended HbA1c target for all patients younger than 18 years is <7.5% (58 mmol/mol).
Type 2 Diabetes Mellitus
Type 2 diabetes is characterized by hyperglycemia usually due to progressive loss of insulin secretion from the beta cell superimposed on background of insulin resistance, resulting in relative insulin deficiency.
- The majority of patients are asymptomatic at presentation, with hyperglycemia noted on routine laboratory evaluation, prompting further testing.
Diagnostic value for T2DM
- Venous plasma glucose, fasting ≥7.0 mmol/L
- Venous plasma glucose, random ≥11.1 mmol/L
- A1c
- Normal <5.7% (39 mmol/mol)
- Pre-diabetes <5.7-6.3% (39-44 mmol/mol)
- Diabetes ≥6.3% (45 mmol/mol)
NOTE: In symptomatic individual, one abnormal glucose value or A1c is diagnostic. However, in asymptomatic individual, a repeat abnormal value is required (2nd A1c is to be done 4 weeks after the first positive test)
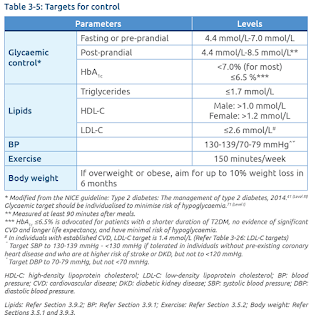
Patients with type 2 diabetes mellitus should be treated with a comprehensive strategy to reduce risks of kidney disease progression and cardiovascular disease, including
- Blood pressure control
- Lipid management
- Dietary control
- Increased physical activity and exercise
- Weight reduction
- Smoking cessation
In the absence of contraindication, metformin is usually the initial pharmacologic therapy for most patients with type 2 diabetes. For patients who do not achieve their goal glycemia on initial oral therapy, there are many medication classes that are available and can be used with metformin:
- Insulin
- Second generation sulfonylurea (e.g. gliclazide, glipizide, glimepiride)
- Alpha-glucosidase Inhibitors (e.g. acarbose)
- Glucagon-like peptide 1 (GLP-1) agonists (e.g. exenatide, liraglutide)
- Sodium-glucose co-transporter (SGLT2) inhibitors (e.g. empagliflozin, dapagliflozin)
- Dipeptidyl peptidase 4 (DPP4) inhibitors (e.g. vildagliptin, sitagliptin, saxagliptin)
Prevention of Type 2 Diabetes Mellitus
Type 2 diabetes mellitus is a progressive metabolic syndrome characterized by variable degrees of insulin resistance and deficiency, resulting hyperglycemia, and complications such as cardiovascular disease, nephropathy, retinopathy, and increased mortality.
Back in university times, we have been taught that lifestyle modification is important to slow us from developing type 2 diabetes
- Dietary therapy including reduced calorie intake and increased intake of whole grains
- Moderate intensity physical activity for at least 150 minutes/week
- 7% weight loss (if overweight)
- Smoking cessation
What's new now is a meta-analysis of randomized trials of metformin for the prevention of type 2 diabetes in high-risk individuals concluded that metformin decreased the incidence of new-onset diabetes compared with standard diet and exercise, but NOT compared with intensive diet and exercise.
Other medications which may reduce the progression to diabetes in patients with prediabetes include:
- Thiazolidinediones (pioglitazone 30-45 mg orally once daily or rosiglitazone 8 mg orally once daily)
- Alpha-glucosidase inhibitors (acarbose, voglibose)
- Orlistat 120 mg 3 times daily
- Thiazolidinediones are limited by adverse effects such as fluid retention, weight gain, heart failure, bone loss, possibly myocardial infarction for rosiglitazone, and possibly bladder for pioglitazone.
- Alpha-glucosidase inhibitors - gastrointestinal side effects and poor long-term compliance.
In contrast, metformin is a relatively inexpensive and safe intervention. Hence, it may be considered, especially if body mass index is ≥35 mg/m2, <60 years old, history of gestational diabetes, and/or elevated HbA1c levels despite lifestyle intervention.
Of note, there is an article that caught my attention: The war on ‘prediabetes’ could be a boon for pharma-but is it good medicine?, 2019.
NOTE: The 2020 American Diabetes Association guidelines state that there is insufficient evidence to recommend the daily use of supplements such chromium, vitamin D, cinnamon or herbs/supplement.
Dietary Supplements
Many studies have investigated dietary supplements for preventing or treating type 2 diabetes or its complications.
Chromium
- Chromium supplementation has been studied for a variety of indications, especially diabetes and weight loss, but clinical studies have shown inconsistent results.
- In 2014, a review of 25 studies, including 1600 diabetic participants, showed that chromium supplements could lead to a decrease in blood sugar levels. However, long term studies are still required.
Alpha-lipoic acid
- A 2016 assessment of treatments for symptoms of diabetic neuropathy that included 2 studies of oral alpha-lipoic acid, with a total of 205 participants, indicated that alpha-lipoic acid may be helpful.
Herbal supplements
- Evidence is lacking for any herbal supplements used to control diabetes or its complications, such as bitter melon, cinnamon, fenugreek, gymnema and milk thistle.
NOTE: Diabetic milk powder often has a lower GI with complex sugar (such as isomaltulose) and added with chromium and inositol to improve blood sugar control.
External Links
- Management of Type 1 Diabetes Mellitus in Children and Adolescents, 2016
- Management of Type 2 Diabetes Mellitus, 2020
- Management of Diabetes in Pregnancy, 2017
- Practical Guide to Inpatient Glycemic Care, 2019
- Practical Guide to Insulin Therapy in Type 2 Diabetes Mellitus
- Standards of Medical Care in Diabetes - 2020 Abridged for Primary Care Providers
- KDIGO CPG for Diabetes Mellitus in CKD, 2020
- NIH - Diabetes and Dietary Supplements





Comments
Post a Comment