SGLT-2 Inhibitors
Introduction
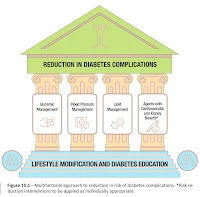
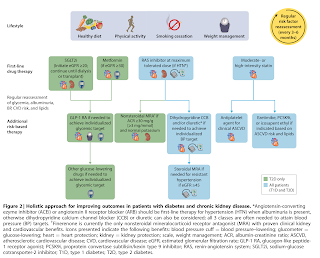
The treatment approach for type 2 diabetes mellitus has undergo a shift from the traditional glucose-centric approach to the new cardiorenal-metabolic approach.
- This change emphasizes a comprehensive approach for reducing the risk of diabetes-related complications.
As a result of this shift, sodium glucose co-transporter 2 (SGLT-2) inhibitors, such as canagliflozin, dapagliflozin and empagliflozin, have emerged as a key player for managing type 2 diabetes.
Mechanism of Action
The SGLT-2 inhibitors act by promoting the glucose excretion into the urine, thereby reducing the concentration of circulating glucose.
- The resulting glycosuria is associated with an osmotic diuresis and salt excretion.
- Furthermore, the osmotic diuretic effect and the caloric loss (from glucose in the urine) also leads to reduction in systolic blood pressure and body weight.
Expected Benefits
Lower blood glucose.
- 0.3-1.0% reduction in HbA1c
- Effect on both fasting and postprandial glucose concentrations
- In short-term placebo-controlled trials, overweight and obese patients treated with SGLT2 inhibitors had modest weight loss (2-3 kg) and slight reduction in BP (3-5 mm Hg); long-term effects are unknown.
Improve cardiovascular outcomes in heart failure patients.
- Reduce the risk of heart failure hospitalization, cardiovascular mortality and all-cause mortality in people with and without cardiovascular disease.
Preserve kidney function in long term.
- An initial drop in eGFR may occur upon SGLT-2 inhibitor initiation, but with subsequent stabilisation.
- KDIGO 2022 advocates initiating an SGLT-2 inhibitors for patients with type 2 diabetes and CKD who have an eGFR ≥20 ml/min per 1.73 m2.
Side Effects
A significant increase in the risk of urinary tract and fungal infections such as candidal vaginitis or balanitis has been reported with SGLT2 inhibition, presumably due to the glycosuria.
- Maintaining good hygiene is important to reduce the chance of this happening.
Natriuresis with diuresis can lead to increased urinary volume, hypotension and dehydration, and is accentuated with concomitant use of thiazide diuretics.
- Make sure patients drink enough water to control thirst in order to avoid dehydration.
Serious, life-threatening, and fatal cases of diabetic ketoacidosis (DKA) have been reported rarely in patients taking an SGLT-2 inhibitor.
- Inform patients of the signs and symptoms of DKA (including rapid weight loss, nausea or vomiting, abdominal pain, fast and deep breathing, sleepiness, a sweet smell to the breath, a sweet or metallic taste in the mouth, or a different odour to urine or sweat), and advise them to seek immediate medical advice if they develop any of these.
- In several cases, the presentation of DKA was atypical with patients having only moderately elevated blood glucose levels, and some of them occurred during off-label use.
- Test for raised ketones in patients with signs and symptoms of DKA, even if plasma glucose levels are near-normal.
- Risk factors for DKA include a low beta cell reserve, conditions leading to restricted food intake or severe dehydration, sudden reduction in insulin, increased insulin requirements due to acute illness, surgery or alcohol abuse.
- Avoid low carbohydrate intake, excessive alcohol intake and keto diets.
- Interrupt SGLT2 inhibitor treatment in patients who are hospitalized for major surgery or acute serious illnesses; treatment may be restarted once the patient's condition has stabilized.
- SGLT-2 inhibitors should be discontinued before any surgery to reduce the risk of ketoacidosis (3 days before with canagliflozin, dapagliflozin and empagliflozin, and 4 days before with ertugliflozin).
- Restart when patient is eating and drinking normally.
- Discontinue treatment if DKA is suspected or diagnosed.
- Do not restart treatment with any SGLT2 inhibitor in patients who experienced DKA during use, unless another cause for DKA was identified and resolved.
Fournier's gangrene, a rare but serious and potentially life-threatening infection, has been associated with the use of SGLT-2 inhibitors.
Canagliflozin may increase the risk of lower-limb amputation (mainly toes) in patients with type 2 diabetes.
- Evidence does not show an increased risk for dapagliflozin and empagliflozin, but the risk may be a class effect.
- Preventive foot care is important for all patients with diabetes.
Drug Interactions
Treatment with a sulfonylurea or insulin
- SGLT-2 inhibitors may increase the risk of hypoglycaemia, may need to reduce dose of sulfonylurea or insulin.
Taking loop diuretics
- SGLT-2 inhibitors have a diuretic effect (osmotic) and may increase the effect of diuretics, particularly loop diuretics.
- Before starting treatment with an SGLT-2 inhibitor, assess volume status and correct volume depletion if necessary; consider reducing the dose of the diuretic in euvolemic patients to avoid further volume depletion.
External Links
- Changing the Concept: From the Traditional Glucose-centric to the New Cardiorenal-metabolic Approach for the Treatment of Type 2 Diabetes, 2021
- KDIGO Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease, 2022
- ADA Standards of Care in Diabetes, 2023
- SGLT2 inhibitors: updated advice on the risk of diabetic ketoacidosis, 2016
- SGLT2 inhibitors: updated advice on increased risk of lower-limb amputation (mainly toes), 2017
- SGLT2 inhibitors: reports of Fournier’s gangrene (necrotising fasciitis of the genitalia or perineum), 2019
- SGLT2 inhibitors: monitor ketones in blood during treatment interruption for surgical procedures or acute serious medical illness, 2020
- Practical considerations for the use of SGLT-2 inhibitors in the Asia-Pacific countries-An expert consensus statement, 2023

Comments
Post a Comment