Drug Adherence
Introduction
Once, a senior pharmacist shared his personal experience in doing medication management review at patients' home. You will be surprised at the medications stockpiled at home.
- To some patients, although they do not take the medications daily as instructed, but they still come to pharmacy monthly to pick up medications.
- It is as if they are having a proper medical treatment when they are only paying visits to clinic and pharmacy appointments.
Key Definitions
‘Compliance’ is defined as the extent to which the patient’s behaviour matches the prescriber’s recommendations.
- It implies that the patient will simply follow the recommendations of the doctor (or other healthcare professional) with little, if any, discussion or negotiation.
‘Concordance’ is a two-way exchange between the healthcare professional and the patient whereby the prescriber and the patient agree therapeutic decisions that incorporate their respective views.
- The patient participates in both the consultation and the decision-making process, and the patient’s preferences and beliefs are considered.
‘Adherence’ is somewhere between compliance and concordance.
- It is the extent to which the patient’s actions meet the prescriber’s recommendations or expectations.
- Ideally, the healthcare professional should accept that the patient’s beliefs, preferences, and prior knowledge influence medicine-taking and should attempt to address this.
- However, adherence interventions are often made after the prescription is written and the patient might not have had much influence on the choice of drug.
- Consequently, pharmacists and other healthcare professionals may have a bigger role in facilitating adherence than doctors.
Factors Reported to Affect Adherence
Numerous studies have attempted to identify the cause of non-adherence and many factors have been identified.
- Ability to attend appointments
- Age
- Beliefs about medicines
- Chaotic lifestyle
- Complexity of regimen
- Concerns about confidentiality
- Cost
- Cultural practices or beliefs
- Depression
- Education status
- Frequency of doses
- Gender
- Health beliefs and attitudes (towards self and others)
- Impact on daily life
- Language (if the patient's first language is different from that of the healthcare professional)
- Literacy
- Manual dexterity
- Past or current experience of side effects
- Satisfaction with healthcare
- Self-esteem
- Side effects
- Socioeconomic status
In summary, the reasons for non-adherence generally fall into 2 categories
- Unintentional (involuntary) or behavioural (e.g. simply forgetting)
- Intentional (voluntary) or cognitive (e.g. concerns about side effects)
NOTE: Pharmaceutical manufacturers tend to concentrate on behavioural factors, producing combination tablets or once-daily version of their medicines, which are supposed easier to take. However, once-daily dosing could, in fact, lead to a worse therapeutic outcome because missing one dose means missing a whole day's therapy. On the other hand, many adherence strategies focus on cognitive issues.
Adherence Support Strategies
Various practical strategies have been used to improve adherence.
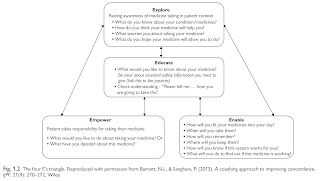
The four E's system can be used to guide the adherence consultations.
NOTE: When questioning the patient about their level of adherence, it is important to do so in a non-judgemental way. Open-ended questions should be used to best evaluate patient understanding.
Case Study - Levothyroxine Challenge Test
At my facility, there was a patient whose levothyroxine dose has been tapered up over the past few years and recently up to 300 mcg TDS, on the basis of levothyroxine malabsorption.
However, based on dispensing record over the past 2 years, I soon realised that the patient has not been complying to pharmacy appointments to collect his medication. It could either be poor medication compliance or patient has been buying medication outside.
NOTE: In general, the maintenance dose of levothyroxine over 300 mcg per day are rarely required. In patients who require high doses, consider poor compliance, malabsorption and/or drug interactions.
I feedback my findings to endocrinologist. He decided to orally assess the patient drug compliance and to admit the patient into ward for a levothyroxine challenge test.
- Serum free levothyroxine level and TSH measurements are assessed before and after 1, 2, 4 and 6 hours using supervised intake.
- An increase in free levothyroxine level is observed with a maximum level within the first 120 min, known to be a normal time interval for absorption by the small intestine.
- After the diagnosis of pseudomalabsoprtion, one should further analyse these patients for a psychiatric condition.
For the case, levothyroxine challenge test result showed an increase of t4 of roughly 100% from baseline. Hence, malabsorption issue is ruled out, but the issue lies with medication adherence.
- A possible solution could be switching to weekly levothyroxine dosing rather than daily administration.
Summary
Non-adherence not only limits the benefit of medicines to patients, but also represent a cost in economic terms (e.g. cost of wasted medicines and costs resulting from patients needing increased healthcare input if their health deteriorates).
- Always consider the issue of patient's medication compliance in medication management, especially when he is on polypharmacy.
External Links
- Gastrointestinal Malabsorption of Thyroxine, 2019
- Pseudomalabsorption of Levothyroxine: A Challenge for the Endocrinologist in the Treatment of Hypothyroidism, 2017
- Medication Adherence to Multi-Drug Regimens, 2012
- Weekly Versus Daily Levothyroxine Tablet Replacement in Adults with Hypothyroidism: A Meta-Analysis, 2021

Comments
Post a Comment