Styes
Introduction
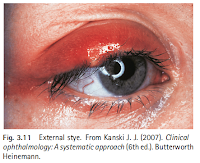
Styes (also called hordeolum) typically present as acute, painful, localized eye swelling that develops over a few days.
- External stye presents as a swollen upper or lower lid, which will be painful and sensitive to touch. A small yellow pus-filled lesion may be visible
- Symptoms of internal styes are similar to those of an external stye, with pain, redness, and swelling being present, although pain is often more severe, and pus-filled lesions are not obvious due to inward growth. If the eyelid is everted, localized swelling should be visible.
NOTE: Staphylococcus aureus is the pathogen implicated in most cases, but hordeola can also be sterile.
Trigger Points
Indicatives of referral
- A chalazion that becomes bothersome to the patient*
- Inward (entropion) or outward (ectropion) of the eyelid margin - requires surgical repair
- Patients with swollen eyelids and associated with feelings of being unwell - suggests orbital cellulitis and blindless is a potential complication
- Middle-aged/elderly patient with painless nodular lesion on or near eyelid - suggests sinister pathology, possibly carcinoma
* A chalazion forms when the meibomian gland becomes blocked. It develops over a number of weeks and initially can cause discomfort but becomes painless. A lump should be clearly visible if the eyelid is everted. A chalazion is self-limiting, although it might take a few weeks to resolve completely. No treatment is needed unless the patient complains that it is particularly bothersome and is affecting vision. Referral in these cases is needed for surgical removal. Because chalazia are not caused by an infection, antibiotics are usually not effective.
Management
Most styes are self-limiting.
- If left untreated, the stye will point and discharge and resolve spontaneously (over 1-2 weeks).
A warm compress applied for 5-10 minutes 3-4 times a day can bring an external stye to a head and, once it bursts, the pain will subside, and the symptoms will resolve.
Although styes are caused by bacterial pathogens, the use of antibiotic therapy is not needed.
- Oral antistaphylococcal antibiotic therapy is indicated if there is accompanying cellulitis.
- Topical application of ocular antibiotics (e.g. chloramphenicol ointment) does not result in speedier symptom resolution, but it might prevent a subsequent staphylococcal infection from a lash lower down.
If, despite management with warm compresses, the lesion does not reduce in size within 1-2 weeks, the patient should be referred to an ophthalmologist for consideration of incision and drainage.


Comments
Post a Comment