Gout
Introduction
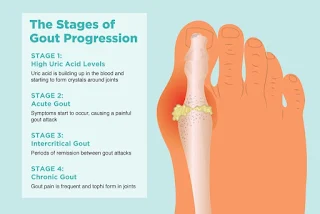
Gout is a common form of inflammatory arthritis characterised by raised uric acid concentration in the blood (hyperuricemia) and the deposition of urate crystals in joints and other tissues.
Risk Factors
- Men
- Elderly - rare in children and pre-menopause women.
- Obesity
- Hypertension
- High consumption of alcohol (particularly beer and spirits), high-purine foods (particularly meat and sea food), leguminous vegetables (like chickpea, peanuts, lentils) and fructose-sweetened drinks
- Medications, such as diuretics, renin-angiotensin system agents, beta-blockers, cyclosporin, tacrolimus, low-dose aspirin (≤325 mg/day)
Clinical Presentation
- Typical episodes of acute gout are characterized by severe pain, erythema, warmth, and swelling of 1 or more joints, peaking within 24 hours and with spontaneous resolution within 7-14 days.
- The first metatarsophalangeal joint (big toe joint) is most commonly affected. Other frequently involved joints include the midfoot, ankles, and knees. Gout is uncommon in axial joints.
- The disease may ultimately progress to chronic tophaceous gout with persistent arthritis, white-yellow intradermal deposits, and frequent recurrent acute attacks.
Gout occurs when the serum uric acid concentration is sufficiently elevated (usually greater than 0.42 mmol/L [7 mg/dL]), and the solubility coefficient of monosodium urate exceeded, long enough for crystals to form in tissues.
- While the presence of hyperuricaemia is important in the diagnosis of gout, patients with acute gout may have a normal serum uric acid concentration.
The gold standard for diagnosis is demonstration of urate crystals (needle-shaped with strong negative birefringence) in synovial fluid or tophus by polarized light microscopy.
Acute Attacks
Although acute attacks are usually self-limited with spontaneous resolution in 1-2 weeks, treatment for an acute attack of gout should be started as soon as possible. Acute attacks are usually treated with either colchicine or high doses of an NSAID (excluding aspirin) or a short course of an oral corticosteroid. The choice of drug depends on factors such as patient preference, renal function, and co-morbidities.
- The most common adverse effects of colchicine, diarrhoea and abdominal cramping, are less likely in patients who receive no more than 1.8 mg in total on the first day, compared with patients receiving higher doses, such as 0.6 mg every one to two hours until symptom relief or intolerance (as was historically employed).
- Consider prescribing a proton pump inhibitor for patients on NSAIDs.
- Combination treatment can be considered for acute attacks of gout in patients with inadequate response to monotherapy.
If NSAIDs or colchicine are unsuitable, an intra-articular injection [unlicensed use] or intramuscular injection of a corticosteroid can be considered. Joint aspiration may also be considered in certain patients with acute monoarticular gout [under specialist guidance].
An interleukin-1 inhibitor, such as canakinumab and anakinra, can be considered for treatment of acute attacks in patients in whom NSAIDs, colchicine and corticosteroids are unsuitable or ineffective.
Long-term Control
All patients with gout should be offered urate-lowering therapy, particularly in those with frequent recurrence of acute attacks of gout (2 or more in a year), the presence of tophi, or signs of chronic gouty arthritis.
- Initiation of long-term urate lowering therapy after a first attack or in patients with infrequent attacks is not recommended.
Urate-lowering therapy should be started at least 2 to 4 weeks after a gout flare has settled, but if flares are more frequent, urate-lowering therapy can be started during a flare.
- The initiation or up-titration of urate-lowering therapy may precipitate an acute attack, and therefore colchicine (0.5-0.6 mg once or twice daily) should be offered as prophylaxis while the target serum urate level is being reached.
- A low-dose NSAID or a low-dose corticosteroid are alternative options if colchicine is unsuitable or ineffective. Consider co-prescribing with a proton pump inhibitor.
- If an acute attack develops during treatment, the urate-lowering therapy should continue at the same dosage and the acute attack treated separately.
NOTE: For most patients, titrate ULT to a target serum uric acid level of ≤6 mg/dL, although some patients may require a level of <5 mg/dL to control symptoms.
Urate-lowering therapy
- Xanthine-oxidase inhibitors
- Allopurinol is recommended as first-line urate-lowering therapy where renal function allows.
- Febuxostat can be used as an alternative when allopurinol is contraindicated or not tolerated.
- Uricosuric drugs, such as probenecid, sulfinpyrazone or benzbromarone
- May be used as urate-lowering therapy in patients who are resistant to or are intolerant of xanthine-oxidase inhibitors; they increase the excretion of uric acid in the urine.
- Uricosuric drugs may also be used in combination with xanthine-oxidase inhibitors in patients who have an inadequate response to monotherapy.
Patients with gout and a history of urolithiasis should be advised to ensure adequate daily fluid intake and avoid dehydration.
- Alkalinisation of the urine with potassium citrate can be considered in recurrent stone formers.
Summary
Before considering pharmacological interventions, dietary control is a fundamental strategy for preventing gout attacks.
- By making specific dietary adjustments, the risk of painful gout flare-ups can be significantly reduced.
Comments
Post a Comment