Tuberculosis
Introduction
Tuberculosis (TB) is a bacterial infection caused by Mycobacterium tuberculosis and is transmitted primarily by inhalation.
- After primary infection, 90% of individuals with intact immunity control further replication control of the bacilli, which may then be cleared or enter a "latent" phase. The person remains asymptomatic, but latent disease has the potential to become active at any time.
- The remaining 10% of individuals develop progressive to primary tuberculosis. It most commonly affects the lungs, although it can affect other parts of the body.
NOTE: In general, individuals with pulmonary and laryngeal TB are infectious (higher risk if sputum smear is positive), whereas those with extrapulmonary TB are regarded as non-infectious.
Clinical Presentation
Pulmonary TB is characterized by its slow onset and initial mild symptoms.
- The cough is chronic in nature and sputum production can vary from mild to severe with associated haemoptysis.
- Other symptoms of the condition are malaise, fever, night sweats and weight loss.
- However, not all patients will experience all symptoms.
On the other hand, symptoms and signs due to extrapulmonary TB vary according to the organs involved and may be non-specific.
Diagnostic Tools
- Chest X-ray
- Sputum acid-fast bacilli (AFB) smear
- Nuclear acid amplification testing (NAA)
- Tuberculin skin test (Mantoux test or TST)
- Interferon-γ release assay (IGRA)
First Line Treatment
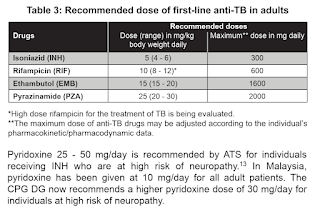
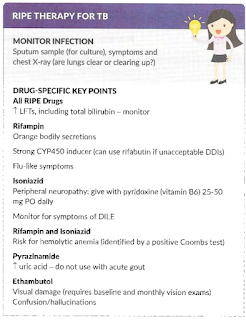
Presently, six-month regimen consisting of 2 months of daily EHRZ (intensive phase), followed by 4 months of daily HR (maintenance phase) is recommended for newly diagnosed pulmonary TB.
- Rifampicin and isoniazid should be taken with an empty stomach to have better absorption.
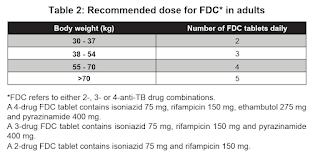
WHO recommends the use of fixed-dose combination (e.g. Akurit-4 and Akurit-2) over separate drug formulations in the treatment of patients with drug-susceptible tuberculosis.
NOTE: Multiples of 18
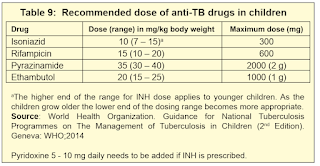
NOTE: The currently available adult anti-TB fixed dose combination tablet is not suitable for use in children <25 kg.
NOTE: Based on WHO operational handbook on tuberculosis, 2022, the upper limit of ethambutol in adult is 25 mg/kg, but daily maximum dose remains 1600 mg.
NOTE: Medication dose requires recalculation every 2 to 4 weeks as children gain weight rapidly, particularly in neonates and young children.
On the other hand, all extrapulmonary TB should be treated with anti-TB for a minimum of 6 months except for bone (including spine) and joint tuberculosis for 6-9 months and tuberculosis for 9-12 months.
Renal Impairment
The clearance of ethambutol and pyrazinamide metabolites are impaired in patients with chronic renal failure when their creatinine clearance falls below 30 ml/min.
- Hence, thrice weekly dosing is recommended in international guidelines.
Conversely, rifampicin and isoniazid do not require dose adjustment in renal failure as they are metabolized by the liver.
Comments
Post a Comment