Warts and Verrucae
Introduction
Cutaneous warts are small, rough growths that are caused by infection of skin cells with certain strains of the human papillomavirus (HPV).
- More than 100 HPV subtypes are known, giving rise to a variety of presentations.
- They can appear anywhere on the skin, but are most commonly seen on the hands and feet.
A verruca (also known as a plantar wart) is a wart on the sole of the foot.
Transmission
HPV is spread by direct skin-to-skin contact or auto-inoculation.
- This means that if a wart is scratched or picked, the viral particles may be spread to another area of skin.
- The incubation period can be as long as 12 months.
Strategies to reduce risk of transmission include
- Cover warts when they are being treated.
- Avoid sharing towels, shoes, or socks.
- Consider HPV vaccination.
Clinical features
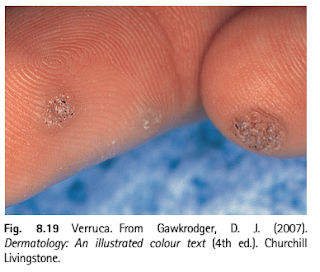
When examined, the wart appears as a raised hyperkeratotic papule with thrombosed black vessels often visible as black dots within the wart.
- They tend to be rough textured and usually less than 1 cm in diameter.
Owing to constant pressure imparted on the sole of the foot, the normal outward expansion of the wart is thwarted and instead grows inward.
- Pressure on nerves can then cause considerable pain, and patients often complain of pain when walking.
NOTE: The presence of capillaries provides a useful distinguishing feature between callouses and verrucae on the feet: if a corn or callous is pared, no such dark points will be seen; instead layers of white keratin will be present.
Management
The best treatment is no treatment.
- Spontaneous resolution is seen in 30% of people within 6 months and two-third of cases within 2 years.
- Despite their self-limiting nature, they are cosmetically unacceptable to many patients, and patients prefer active treatment.
Treatment of viral warts can be more uncomfortable and troublesome than the warts. To get rid of them, we have to stimulate the body's own immune system to attack the wart virus. Persistence with the treatment and patience is essential!
Topical salicylic acid and liquid nitrogen cryotherapy have the best evidence for efficacy.
- The former is less painful.
- Plantar warts have poorer outcomes than common warts elsewhere.
Wart paints containing salicylic acid or similar compounds
- Acts by softening and destroying the lesion by chemically burning, thus mechanically removing affected tissue.
- Salicylic acid is often combined with other ingredients, in particular lactic acid. However, there is no evidence to support greater efficacy when lactic acid (or another ingredient) is added.
- 70% of warts resolve within 12 weeks (i.e. 3 months) of daily applications
- Soften the wart by soaking in a bath or bowl of hot soapy water.
- Rub the wart surface with a piece of pumice stone or emery board.
- Apply wart paint accurately, allowing it to dry.
- Cover with plastic or duct tape.
- If the wart paint makes the skin sore, stop treatment until the discomfort has settled, the recommence as above. Take care to keep the chemical oof normal skin.
- Protection of the surrounding skin can be achieved by applying a layer of petroleum jelly to prevent the treatment from making contact with healthy skin.
NOTE: Tools used for paring down warts (e.g., nail file, pumice stone, etc) should not be reused on normal skin or nails and should not be shared with others.
Cryotherapy
- Is normally repeat at 1-3 week intervals.
- It is uncomfortable and may result in blistering for several days or weeks.
- Success is in the order of 70% after 3-4 months of regular freezing.
- A hard freeze using liquid nitrogen might cause a permanent white mark or scar. It can also cause temporary numbness.
NOTE: Efficacy of OTC single-use cryotherapy treatments may vary based on size of the wart, type of applicator on the product, and ease of use at home. It may not be as effective as liquid nitrogen as it does not get as cold as liquid nitrogen (OTC products typically reach -57°C vs. -196°C with liquid nitrogen).
The best approach to treatment-refractory warts is unclear. Therapies include
- Topical immunotherapy with contact allergens, such as squaric acid dibutylester (SADBE), dinitrochlorobenzene (DNCB) and diphenylcyclopropenone (DPCP)
- Intralesional bleomycin
- Pain from bleomycin injection typically lasts for one to two days and is followed by tissue necrosis with the formation of a black eschar.
- Treatment with bleomycin is not recommended for children, pregnant women, immunosuppressed patients, or patients with vascular disease because of systemic absorption.
- Topical or intralesional fluorouracil
These interventions have limited or conflicting evidence for efficacy and are often used in conjunction with wart paring and topical salicylic acid.
- Cantharidin
- Imiquimod
- FDA approved for the treatment of anogenital warts, but may not be effective for clearing cutaneous warts.
- Trichloroacetic acid
- Duct tape
- Pulse dye laser
- Intralesional immunotherapy with antigens
- Antigens used in trials include measles, mumps, and rubella [MMR], Candida, Trichophyton, tuberculin purified protein derivative (PPD), and Bacillus Calmette Guerin (BCG).
- Surgical removal (e.g. removal or curettage with or without electrodessication)
- Scarring often limits use in cosmetically sensitive skin
- Oral cimetidine
Summary
While wart lesions typically resolve once immunity to the infecting virus is sufficiently high, many patients (and parents) opt for active treatment but often discontinue it prematurely, driven by an expectation of a rapid cure.
External Links
- UpToDate - Cutaneous Warts (Common, Plantar and Flat Warts)
- Treatment of common warts with high-potency (26%) salicylic acid, 1988
- Topical treatments for cutaneous warts, 2012
- Management of cutaneous viral warts, 2014
- Efficacy and Safety of Three Cryotherapy Devices for Wart Treatment: A Randomized, Controlled, Investigator-Blinded, Comparative Study, 2018
- Efficacy and tolerability of intralesional bleomycin in dermatology: A systematic review, 2020

Comments
Post a Comment