Thyroid Disorders
Introduction
The thyroid gland secretes 3 main hormones
- Thyroxine (T4)
- Tri-iodothyronine (T3)
- Calcitonin - involved in the control of plasma calcium
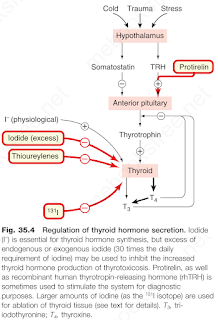
* Thyroid-stimulating hormone (TSH; thyrotrophin)
The majority of the secreted hormone is T4. This is converted into the (three- to five-fold) more active species, T3, in a tissue-specific manner. Both hormones are critically important for normal growth and development and for controlling energy metabolism.
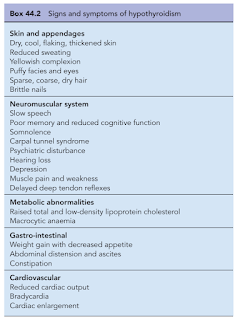
Hypothyroidism
In hypothyroidism, there is a deficiency in T4 and consequently, an elevation in TSH.
Hypothyroidism occurs more commonly in females (~80% of cases). The incidence increases with age. The most common cause of hypothyroidism is Hashimoto's disease, an autoimmune condition in which a patient's own antibodies attack the thyroid gland.
The goals of treatment are to resolve symptoms, normalize TSH and avoid over-treatment. Levothyroxine (T4) is usually the drug of choice for hypothyroidism, except in myxoedema coma, where T3 may be used in the first instance.
- A consistent preparation (i.e. the same formulation and manufacturer) is preferred to minimize variability form refill to refill.
- Levothyroxine should be taken with water consistently at least 30-60 minutes before breakfast or at bedtime (at least 3-4 hours after the last meal) for consistent absorption.
- Do not administer within 4 hours of calcium- or iron-containing products.
Hyperthyroidism
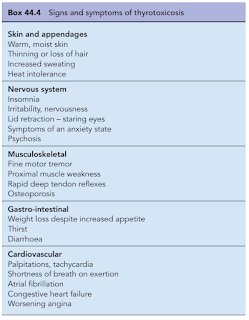
Hyperthyroidism is defined as the production by the thyroid gland of excessive amounts of thyroid hormones. Thyrotoxicosis refers to the clinical syndrome associated with prolonged exposure to elevated levels of thyroid hormone.
- FT4 is high and TSH is low, and symptoms are nearly opposite of those seen in hypothyroidism.
The most common cause of hyperthyroidism is Graves' disease, which most commonly occurs in females ages 30-50 years.
- Graves' disease is an autoimmune disorder and results from production of an abnormal immunoglobulin G that is able to occupy the TSH receptor on the thyroid follicular cell, causing cell division and stimulating thyroid hormone secretion.
Three forms of therapy are available, including antithyroid drugs, radioactive iodine and surgery. There is no general agreement as to the specific indications for each form therapy, and none of them is ideal, because all are associated with both short- and long-term sequelae.
- Neither surgery nor radioactive iodine should be given until the patient has been rendered euthyroid because of the risk of inducing a thyroid crisis.
- With any option, the patient can be treated with beta blockers first for symptom control (to reduce palpitations, tremors and tachycardia).
Anti-thyroid medications, e.g. propylthiouracil, carbimazole
- The most common adverse effect of antithyroid treatment is rash and arthropathy (5%) and less commonly agranulocytosis, hepatitis, aplastic anaemia and lupus-like syndromes. Overall, serious effects such as these occur in approximately 0.3% of patients treated. These side effects usually occur during the first 6 weeks of treatment, but this is not invariable. Cross-sensitivity between carbimazole and propylthiouracil is around 10%, and the patient can often be safely changed to the alternative agent if an adverse event occurs.
- Carbimazole is associated with congenital defects, including aplasia cutis of the neonate, therefore propylthiouracil remains the drug of choice during the first trimester of pregnancy. In the second trimester, consider switching to carbimazole because of the potential risk of hepatotoxicity with propylthiouracil. Both propylthiouracil and carbimazole cross the placenta and in high doses may cause foetal goitre and hypothyroidism - the lowest dose that will control the hyperthyroid state should be used.
Radioactive iodine (131I)
- Antithyroid drugs must be withdrawn 1 week prior to radioiodine is given and should not be restarted for at least 3 days afterwards (otherwise the isotope will not be trapped by the thyroid).
- Because the ablative effect of radioiodine usually commences within 2-3 months, many patients with mild or moderate disease will not need to restart their drug treatments, although close patient monitoring is required.
- Patients with severe thyrotoxicosis should restart their antithyroid drugs on day 3. Treatment is then withdrawn periodically to assess the effects of the radioiodine.
- 24-90% develop hypothyroidism over their lifetime, depending on dose given.
- Contraindicated during pregnancy and lactation.
Surgery (Thyroidectomy)
- The patient with hyperthyroidism to be treated surgically should first be rendered biochemically euthyroid whenever possible, but occasionally surgery needs to be performed as a semi-urgent procedure. This may require urgent patient preparation with a combination of antithyroid drugs and β-blockers, and iodide given as Lugol's solution.
- 6-75% develop hypothyroidism over their lifetime, dependent on the amount of remnant tissue.
Comments
Post a Comment