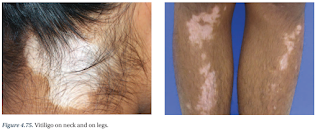
Vitiligo
Introduction
Vitiligo is a skin disorder characterized by an absence of pigmentation due to loss of functioning melanocytes.
- It usually starts between the ages of 10 and 30 years, and tends to be chronic and progressive.
The disease is most disfiguring in darker skin types and can have a marked psychological impact (e.g. stigmatization, isolation and low self-esteem).
- Family support, counselling and cognitive behavioural treatment can be of benefit.
Many patients have a family history of vitiligo and a personal or family history of other autoimmune disorders.
Management
For all patients, recommend avoidance of potential provoking factors, such as stress, sunburn, mechanical or chemical irritation.
- Wear protective clothing to minimize skin injury
- Sun protection
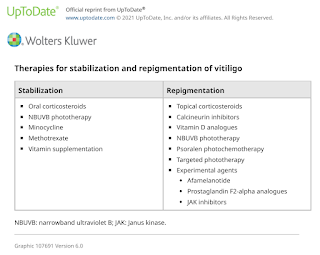
Although there is no cure for the disease, the available treatments may halt the progression of the disease and induce varying degrees of repigmentation.
Treatment modalities (topical, systemic or light-based therapies) are chosen in the individual patient, based on
- Disease severity
- Disease activity (stable versus progressive disease)
- Patient preference (including cost and accessibility)
- Response evaluation
For localized disease (<10% of body surface area), consider a potent or very potent topical steroid or topical calcineurin inhibitors for 2 to 3 months.
- Topical ruxolitinib 1.5 % cream (a Janus kinase inhibitor) can be used as first- or second-line treatment of nonsegmental vitiligo affecting ≤10 percent of the body surface area (BSA), including the face, in patients ≥12 years.
Whereas, for disseminated disease (affecting multiple anatomic sites but overall involvement of <5-10% of the total body surface area), first-line treatment is phototherapy with narrowband ultraviolet B.
- The use of topical corticosteroids may be unpractical.
Depigmentation of residual pigmented areas with monobenzyl ether of hydroquinone (monobenzone) can be offered for patients with recalcitrant disease that does not respond to repigmentation regimens and for those with extensive vitiligo who do not desire undergoing repigmentation treatments.
- Depigmentation therapy may require 1 to 3 years to achieve optimal outcomes.
- Monobenzone should never be used as a lightening agent in disorders of pigmentation other than vitiligo. It will induce vitiligo in normal individuals.
Camouflage, if desired, can be beneficial during treatment or as an alternative to treatment for patients with vitiligo affecting exposed areas, such as the face, neck and hands.
- Camouflage products include foundation-based cosmetics and self-tanning products containing dihydroxyacetone (DHA).
- DHA-based products provide lasting colour for up to several days and are not immediately rubbed off onto clothing.
Dietary Supplements
Oral supplementation with antioxidants and vitamins is often used as an adjunctive treatment for vitiligo, usually in combination with phototherapy. However, there is limited evidence from high-quality studies to support their use.
- High-dose vitamin supplementation, vitamin C, vitamin B12 and folic acid
- Alpha-lipoic acid
- Ginkgo biloba
- Oral extracts of Polypodium leucotomos
Prognosis
Vitiligo is a chronic disease with a highly unpredictable course.
- Early-onset vitiligo appears to be associated with involvement of a greater body surface area and increased rate of disease progression.
- Despite treatment, most patients experience alternating periods of pigment loss and disease stability for their entire life.
- Occasionally, patients may experience spontaneous repigmentation.
Externa Links
- UpToDate - Vitiligo: Management and prognosis
- Treatment of vitiligo vulgaris with narrow-band UVB and oral Polypodium leucotomos extract: a randomized double-blind placebo-controlled study, 2007
- Depigmentation therapies in vitiligo, 2012
- Guidelines for the management of vitiligo: the European Dermatology Forum consensus, 2012
- The Vitiligo Working Group recommendations for narrowband ultraviolet B light phototherapy treatment of vitiligo, 2017
- The Role of Diet and Supplements in Vitiligo Management, 2017
- Ginkgo biloba extract protects human melanocytes from H2 O2 -induced oxidative stress by activating Nrf2, 2019
Comments
Post a Comment