Healthcare Systems
Introduction
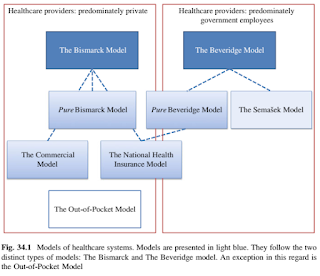
Various healthcare systems have developed around the world.
- They all use, to a larger or smaller extent, elements of The Bismarck Model and The Beveridge Model.
- The Out-of-Pocket Model represents another possible approach.
NOTE: Universal health coverage, as defined by WHO, requires all people to have access to needed health services without the risk of financial hardship associated with accessing services.
The Bismarck Model
The Bismarck model is a social insurance model where it is compulsory for all citizens to belong to an insurance fund.
- Insurance agencies have a high level of autonomy, which means that the finances cannot be used for other purposes than health care. They are run as non-profit organizations and are required to accept all citizens without discrimination.
- Healthcare providers tend to be largely private.
- The system is based on the demand/supply basis with the possibility to freely choose among different insurance programmes.
- The premiums are based on risk assessments and the insurances can also refuse the request for insurance.
National Health Insurance Model is a single-payer, state-run insurance programme, which is compulsory for all citizens.
- Payroll contributions are often supplemented by general taxation or other public funds.
- Predominantly private facilities and providers of health care
The Beveridge Model
In the Beveridge Model, health care is financed by the government (single-payer system) through tax payments.
- Many healthcare facilities are owned by the government, and the healthcare workers are government employees.
The Out-of-Pocket Model
The Out-of-Pocket Model is based on direct payments from patients to healthcare workers at the time of treatment.
- Such a system does not present a systematic approach that would assure health care to all citizens in need.
Malaysia: Health White Paper
The Health White Paper, which was first tabled in the Parliament on 14 June 2023, is a comprehensive proposal to revamp the country's healthcare system for a higher quality, more sustainable and resilient health system in stages over a 15-year period.
The policy paper depicted the existing health system gaps and challenges, which includes
- Ageing population
- Rising burden of non-communicable diseases
- Hidden epidemic (mental health)
- Persistent problem of communicable diseases (e.g. COVID-19, polio, measles)
- Constraints in health funding
- Constraints in human resources and infrastructures (e.g. old health facilities and equipment, shortage of health personnel)
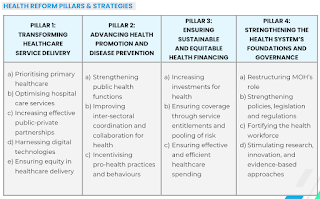
The Health White Paper rests on 4 pillars.
Reforms under these 4 pillars include
- Setting up a national disease control centre.
- Reviewing fees at all public hospitals and clinics.
- Providing incentives to promote a healthy lifestyle.
Summary
Citing the rising cost of healthcare at private hospitals, insurance providers have sent medical insurance price revision notices to policyholders.
- What has surprised the public more is the possibility of this becoming an annual event, as current premium increases still do not seem to align with the high claim rates.
- To illustrate, medical insurance premiums are expected to rise by 40-70% in 2025.
Despite holding medical insurance policies with coverage ranging from 1 to 3 million, the increase in health insurance premiums has burdened the general public, making it difficult for them to afford coverage and leading some to cancel their policies.
- Consequently, with ongoing inflation, many will likely rely on employer-provided insurance or turn to government healthcare facilities.
- The fallout from these cancellations is likely to place an additional strain on Malaysia's already overburdened public healthcare system.
- With public hospitals already struggling with overcrowded wards, long waiting times, and overworked healthcare professionals, an influx of former private insurance policyholders will further compromise the quality and accessibility of public healthcare services.
Some argue that the rising cost of private insurance is due in part to different and non-transparent medical charges levied by private hospitals.
- They claim that patients who pay out-of-pocket may be charged differently compared to those with insurance and guarantee letters.
- This raises concerns about whether the premium increases truly reflect rising healthcare costs or are a means of profiteering by private hospitals and insurance companies at the expense of consumers.
Strategies such as fee regulation, cost-sharing mechanisms, price controls and transparent billing practices are necessary to create a more equitable healthcare system.
External Links
- Global Healthcare: 4 Major National Models And How They Work, 2020
- Understanding Malaysia’s Healthcare System
- Healthcare Systems
- Malaysia Health White Paper
- Health White Paper aims to tackle Malaysia's healthcare issues systematically, 29 Aug 2022
- White Paper: MoH moots raising public healthcare fees for those with means, but keep safety net for low-income groups, 13 June 2023
- Skim Perubatan MADANI
- Majority Health Insurance Premiums Rose Up To 20% This Year: Bank Negara, 2024
- Medical insurance premiums reportedly set for 40-70% rise, 2024
- IJN Ordered To Switch Government Patients To Generic Drugs, 2024
- IJN seeks 10-40pc fee increase for MoH patients amid rising healthcare costs, 2024
- How Much Will It Cost MOH To Continue Funding Pensioners At IJN?, 2024
- Addressing rising insurance costs: Insights from global healthcare, 2024
- MOH says no U-turn on mandatory medicine price display, 2024
- Public riled up as UMMC's patient fees shoot up, 2025
Healthcare is such a crucial topic, especially in today’s world where access to quality care can make all the difference. It’s great to see more discussions around the importance of preventive care, mental health, and affordable options for everyone.
ReplyDeleteAn insightful look at healthcare systems! Choosing the right Health Insurance Plans plays a vital role in ensuring accessible and affordable medical care for all.
ReplyDelete