Drug Overdose and Poisoning
Introduction
Drug poisoning can produce a wide range of symptoms and clinical findings. Presentation depends upon
- The agent ingested
- Whether ingestion is acute or chronic
- Baseline prescription medications a patient may be taking
- The ingestion involves a single drug or several coingestants
NOTE: If the poisoning is intentional, patients may not tell the truth about what has been taken. Refer all patients with presence of psychiatric disorder or high suicide risk to psychiatrist.
General Poisoning Management
Only a few poisons (such as opioids, paracetamol and iron) have specific antidotes; few patients require active removal of the poison. In most patients, treatment is directed at managing symptoms as they arise.
Management includes supportive measures, decontamination, elimination enhance and antidotes (if available).
- Prevent absorption (e.g. GI decontamination with activated charcoal gives within 1 hour of overdose ingestion),
- Chelate and neutralize the poisons directly (e.g. DigiFab that binds to Digoxin)
- Accelerate detoxification (e.g. N-acetylcysteine that acts as a glutathione substitute that combines with hepatotoxic paracetamol metabolites and detoxifies them)
- Reduce toxic conversion (e.g. Ethanol which inhibits the metabolism of methanol to toxic metabolites by competing for the same enzyme (alcohol dehydrogenase)
- Competes for receptor site (e.g. Naloxone which antagonizes the effects of opioids at stereospecific opioid receptor opioid sites)
- Blocks the receptor site (e.g. Atropine which antagonizes the effects of the anticholinesterase agents, such as organophosphorus compounds at the muscarinic sites).
NOTE: Do not deprive a hypoxic patient of oxygen except for paraquat or diquat (herbicides) inhalation or ingestion (oxygen radicals increase morbidity).
Available Antidotes
Antidotes are substances that stop the harmful effects of the poison or overdosed drug.
- Anticholinergics - Physostigmine
- Apixaban - Andexanet alfa
- Arsenic - Dimercaprol, Succimer/dimercaptosuccinic acid (DMSA)
- Benzodiazepine - Flumazenil (for respiratory arrest)
- Cyanide - Hydroxocobalamin
- Dabigatran - Idarucizumab
- Digoxin - Digoxin Immune Fab (DigiFab)
- Fluoropyrimidine (e.g. fluorouracil, capecitabine) - Uridine triacetate
- Gold - Dimercaprol
- Heparin - Protamine sulphate
- Iron - Desferrioxamine B Methanesulphonate, deferiprone, deferasirox
- Lead - Dimercaprol, D-penicillamine, Succimer/dimercaptosuccinic acid (DMSA)
- Local anaesthetic (e.g. bupivacaine, mepivacaine, ropivacaine) - Fat emulsion 20%
- Malignant hypothermia - Dantrolene sodium
- Mercury - Dimercaprol, Succimer/dimercaptosuccinic acid (DMSA)
- Methanol - Ethanol, Fomepizole
- Methemoglobinemia from topical benzocaine, dapsone, nitrates or sulphonamides - Methylene blue
- Methotrexate - Leucovorin
- Naphthalene - Methylene blue
- Neuroleptic malignant syndrome - Bromocriptine
- Neuromuscular blockade induced by rocuronium or vecuronium - Sugammadex
- Nondepolarizing neuromuscular blockade - Neostigmine
- Opioids - Naloxone
- Organophosphate - Atropine, Pralidoxime
- Paracetamol - N-Acetylcysteine
- Paraquat - Fuller's Earth
- Rivaroxaban - Andexanet alfa
- Serotonin syndrome - Cyproheptadine
- Thallium - Prussian blue
- Valproate or topiramate induced hyperammonaemia - Levocarnitine
- Warfarin - Vitamin K (Phytomenadione)
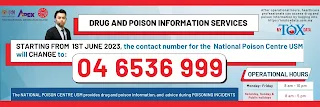
Malaysia National Poison Centre (NPC)
Starting from 1st June 2023, the contact number for the Malaysia National Poison Centre will be changed to +604-6536999. This number can be used by healthcare professional and individuals seeking drug and poison information.
- Additionally, after operational hours, healthcare professionals can access drug and poison information by logging into https://mytoxdata.usm.my.

Comments
Post a Comment