Ramadan and Diabetes
Introduction
During Ramadan, fasting is obligatory for all Muslim adults (including adolescents that have reached the age of puberty), with certain groups exempted, such as those who are suffering with illness (including diabetes).
Studies have showed that many diabetic patients choose to fast despite being exempted.
- A population-based study of diabetes and its characteristics during the fasting month of Ramadan in 13 countries: results of the epidemiology of diabetes and Ramadan 1422/2001 (EPIDIAR) study, 2004
- Patterns of Diabetes Care Among People with Type 1 Diabetes During Ramadan: An International Prospective Study (DAR-MENA T1DM), 2020
- The DAR 2020 Global survey: Ramadan fasting during COVID 19 pandemic and the impact of older age on fasting among adults with Type 2 diabetes, 2021
Hence, it is important the decision is made on an individual basis and in consultation with the patient's treating physician, taking in to account he severity of illness and the level of risk involved.
- Fasting in diabetes during Ramadan may be associated with adverse outcomes in certain individuals which include hypoglycaemia, hyperglycaemia/ketoacidosis, dehydration and thrombosis.
IDF-DAR Risk Stratification
Risk levels and associated recommendations
- High risk = should not fast.
- Moderate risk = advised not to fast.
- Low risk = should be able to fast.
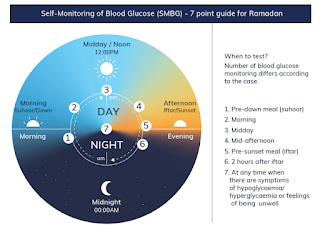
Frequent SMBG or Continuous Glucose Monitoring (CGM)
There is a misconception held by some Muslim communities that pricking the skin for blood glucose testing invalidates the Ramadan fasting. Hence, it should be strongly emphasized that this is not the case.
Patients are advised to monitoring their plasma glucose and most importantly when symptomatic of hypoglycemia. The frequency of SMBG depends on risk factors and current medications.
- For those at moderate or low risk, this may be once or twice a day.
- Those at high or very high risk should check their plasma glucose levels several times a day.
- Patients on insulin and/or sulfonylureas may need to monitor their plasma glucose levels more frequently.
Criteria to Terminate Fasting
CPG Management of Type 2 Diabetes Mellitus, 2020- Blood glucose <3.3 mmol/L at any time during fast.
- Blood glucose <3.9 mmol/L within first few hours of fasting; in particular, if on sulfonylureas, meglitinides or insulin
- Blood glucose >16.7 mmol/L at any time during fast.
- When experiencing symptoms of hypoglycemia, or severe dehydration, e.g. giddiness, syncope or confusion.
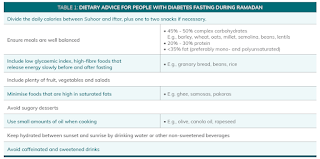
Healthy Diet and Physically Active Lifestyle
The fasting and feasting nature of Ramadan can encourage the consumption of large, carbohydrate-heavy meals, and sugary drinks and treats that can impact blood glucose levels potentially increasing the risk of complications in people with diabetes.
Recommendations for Sahur (pre-dawn meal)
- Should never be omitted.
- Should consist of a balanced meal with adequate carbohydrate.
- To be taken as late as possible, just before Imsak (dawn).
- Intake of salty foods should be avoided to reduce risk of dehydration.
Recommendations for Iftar (breaking of fast at sunset)
- It should not be delayed.
- Intake of high-sugar foods should be avoided. However, 1-2 kurma (dates) at the start of Iftar following the practice of the Prophet (Sunnah) may be taken as part of carbohydrate exchange.
- Sufficient fluid should be taken to replenish fluid loss during the day. Aim for 8 glasses of fluid a day.
- The main meal is encouraged after the performance of Maghrib prayers.
- Supper after Tarawih (supererogatory prayers) can be considered as a pre-bed snack.
Rigorous exercise should be avoided, particularly during the last hours of fasting (before sunset) because it may lead to an increased risk of hypoglycaemia and/or dehydration.
- The timing of exercise is preferably performed 1-2 hours after Iftar.
Medication Adjustments during Fasting
The preferred oral glucose lowering therapies are those which have low risk of hypoglycaemia.
- SGLT2-i has lower risk of hypoglycaemia, but are associated with some safety concerns in particular, dehydration.
The principles of oral glucose lowering therapies modifications are
- The non-fasting morning dose should be taken during Iftar, and the non-fasting evening dose should be taken during Sahur; and
- The dose of glucose lowering agents may be maintained or reduced depending on risk of hypoglycemia.
|
Regimen |
Pre-dawn meal (Sahur) |
Sunset meal (Iftar) |
|
Alpha-glucosidase inhibitors |
No
change |
No
change |
|
Biguanides (metformin) |
No
change |
No
change |
|
Dipeptidyl peptidase-4 inhibitors |
Switch
timing to Iftar |
|
|
Meglitinides |
No
change |
No
change |
|
Sulfonylureas |
Glibenclamide: reduce/omit Gliclazide: reduce/omit/switch
timing to Iftar Gliclazide MR: switch timing to Iftar/may need to reduce dose Glimepiride:
switch timing to Iftar/may need to reduce dose |
No
change |
|
Sodium-glucose transporter 2
inhibitors |
Switch
timing to Iftar |
|
|
Thiazolidinediones |
No
change |
|
Non-insulin anti-diabetic injectables
|
Regimen |
Pre-dawn meal (Sahur) |
Sunset meal (Iftar) |
|
Glucagon-like peptide-1 receptor
agonists |
Liraglutide
and exenatide: No dose modification is required, and injection
should be given at Iftar. Lixisenatide
and Dulaglutide: Data are lacking. |
|
Insulin therapy
- Insulin use during prolonged fasting carries an increased risk of hypoglycaemia.
- Use of insulin analogues is preferred over regular human insulin due to a number of advantages that include fewer episodes of hypoglycaemia and smaller post prandial glucose rise after sunset meal (Iftar)
- Individualised adjustments of insulin dose and timing will need to be implemented when fasting during Ramadan. In those who are prone to developing hypoglycaemia, insulin analogues may be a better alternative.
|
Insulin regimen |
Type 1 diabetes mellitus |
Type 2 diabetes mellitus |
|
Basal insulin only |
Not
applicable. |
Basal
Insulin to be taken at bedtime or after Iftar. May
need dose reduction if there is a risk of daytime hypoglycemia. Patients
who are well/tightly controlled suggest dose reduction of 15-30%. |
|
Premixed insulin once daily |
Not
applicable. |
Inject
usual dose at Iftar. |
|
Premixed insulin twice daily |
Reverse
doses - Morning dose given at Iftar and evening dose at Sahur. Insulin
dose at Sahur reduced by 20-50% to prevent daytime hypoglycemia. |
Reverse
doses - Morning dose given at Iftar and evening dose at Sahur. Iftar:
Give morning dose - dose may need to be adjusted. Sahur:
Insulin dose reduced by 20-50% to prevent daytime hypoglycemia. OR Change
to short/rapid acting. * *
Lafe afternoon hypoglycemia may occur. |
|
Basal
bolus insulin Basal Insulin Bolus/Prandial Insulin |
Taken
at bedtime or any time after Iftar. May require a dose reduction if there is
daytime hypoglycemia. Sahur:
Usual pre-Ramadan breakfast or lunch dose. Adjust according to carbohydrate
intake. May require dose reduction to avoid post meal hypoglycemia. Lunch:
Omit. Iftar:
Usual pre-Ramadan dinner dose. Dose adjustment according to carbohydrate
intake. Insulin should be taken before the main meal. *
Total insulin requirement for Type 1 diabetics who are on basal bolus insulin
regimen while fasting during Ramadan may require dose reduction by 15-30% of
their pre-Ramadan dose requirements. |
|
|
Insulin Pump |
Basal
insulin rate: Unchanged or may require reduction of up to 25%. Prandial
bolus: According to individualized insulin-to-carbohydrate ratio (ICR). |
|
Reminder
It should be stressed to the patient that a safe fast one year does not automatically make them a low risk for the next year due to the progressive nature of the disease.

Comments
Post a Comment