Addison Disease
Introduction
Primary adrenal insufficiency, or Addison's disease, is a chronic, rare condition which occurs when the adrenal glands fail to produce any or a high enough level of
- Mineralocorticoids, e.g. aldosterone
- Glucocorticoids, e.g. cortisol
- Adrenal androgens, e.g. dehydroepiandrosterone (DHEA)
Adrenal insufficiency most often involves the destruction of all regions of the adrenal cortex.
- In developed countries, autoimmune dysfunction is responsible for most cases (80-90%), whereas tuberculosis predominates as the cause in developing countries.
- It is more common in women than men, and onset tends to be between the ages of 30-50 years of age.
Medications may also cause primary adrenal insufficiency by
- Inhibit cortisol synthesis (e.g. ketoconazole)
- Accelerate cortisol metabolism (e.g. phenytoin, rifampin, phenobarbital)
Secondary insufficiency is characterized by reduced glucocorticoid production secondary to ACTH levels.
Symptoms
The symptoms of adrenal insufficiency are non-specific.
- Appetite loss, unintentional weight loss
- Discolouration of the skin
- Dehydration
- Increased thirst and need to urinate frequently
- Salt, soy sauce or liquorice cravings
- Oligomenorrhoea (irregular or infrequent periods in women)
- No energy or motivation (fatigue, lethargy), low mood
- Sore/painful, weak muscles and joints.
Further symptoms can occur gradually over months or years.
- Chronic exhaustion leading to depression
- Diarrhoea
- Nausea and vomiting
- Postural hypotension, which can lead to dizziness and fainting
- Reduced libido, especially in women
Chronic Management
Once diagnosis of primary adrenal insufficiency is confirmed,
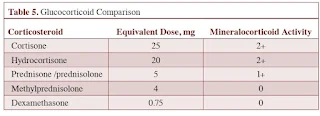
- Glucocorticoid replacement therapy with hydrocortisone is recommended in all patients.
- Hydrocortisone is considered as the first-line drug because
- It is the closest imitation of what the body produces.
- It is absorbed into the body quicker than other corticosteroids.
- It can be easily measured in the bloodstream, making monitoring of dosage easier.
- For hydrocortisone or cortisone, the majority of the dose (67%) is given in the morning and the remainder (33%) is given 6 to 8 hours later to duplicate the normal circadian rhythm of cortisol production.
- Once daily dexamethasone or prednisolone can also be used but are less common.
- Monitoring parameters should include body weight, postural blood pressures, subjective energy levels, and signs of frank glucocorticoid excess.
- Mineralocorticoid replacement with fludrocortisone is recommended in all patients with confirmed aldosterone deficiency.
- Titrate dose individually based on blood pressure, serum sodium and potassium concentration, and plasma renin activity.
- Some patients may not require fludrocortisone once stabilised on hydrocortisone.
- The dose of fludrocortisone may need to be increased when the patient is exposed to high temperatures and/or humidity - this is to compensate for the increased salt loss from sweating.
- Consider trial of dehydroepiandrosterone (DHEA) in women with primary adrenal insufficiency who have low libido, depressive symptoms, and/or low energy levels despite receiving optimized glucocorticoid and mineralocorticoid replacement therapies.
Increased doses of glucocorticoids are required in patients experiencing medical or surgical stress to prevent adrenal crisis.
- Sick-day rules: Double or triple the glucocorticoid replacement dose.
- Life-threatening symptoms such as severe dehydration, hypotension, hypovolaemic shock, altered consciousness, seizures, stroke or cardiac arrest may develop; if left untreated, adrenal crisis may lead to death or permanent disability.
thanks
ReplyDelete