Thalassemia
Introduction
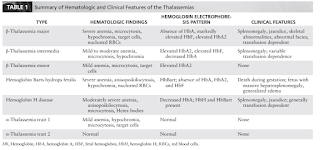
Thalassemia syndromes encompasses a spectrum of haemoglobin disorders that arise from impaired production of globin chains.
- A normal haemoglobin consists of two α chain (encoded by two closely linked genes on chromosome 16) and two β chain (encoded by a single gene on chromosome 11).
Pathophysiology
The imbalance of globin production is variable, and the degree of accumulation of the unpaired globin chains is directly related to the severity of the disease phenotype.
In general,
- α-thalassemia occurs as a result of gene deletion.
- α-thalassemia trait 2 (loss of one α globin gene [αα/α−]);
- α-thalassemia trait 1, also referred to as α-thalassemia minor (loss of two α globin genes [αα/− − or α−/α−]);
- Hemoglobin H (HbH) disease (loss of three alleles [α−/− −]); and
- Hemoglobin Barts hydrops fetalis (loss of all four α globin loci [− −/− −]).
- β-thalassemia occurs as a result of mutations
- Subdivided into major, intermedia, and minor types.
The hallmark of thalassemia is anaemia that is a consequence of both increased destruction (i.e. haemolysis) and decreased production (i.e. ineffective erythropoiesis).
Iron overload is one of the primary causes of morbidity. Even without transfusion, the long-standing anaemia, however mild, leads to increased iron absorption in the gut and eventual chronic iron overload. Excessive iron deposition causes devastating damage to multiple organs, particularly affecting the heart, liver, and endocrine organs.
Management
The key intervention for the management of β-thalassemia major is chronic transfusion therapy.
- In particular, during the first decade of life, regular transfusion results in improvements in hepatosplenomegaly, skeletal abnormalities, and cardiac dilation.
- Patients typically require 1 to 3 units of packed RBCs every 3 to 5 weeks.
- Common treatment targets include pretransfusional Hb level of 9-10 g/dL and posttransfusional Hb level 13-14 g/dL.
Iron Chelation Therapy
- Because of increased iron absorption and long-term transfusion therapy, iron overload develops.
- Historically, deferoxamine (Desferal) has been the most widely used chelator. However, compliance with daily injections has been a particular problem.
- Deferiprone (Ferriprox) was the first orally active chelator to be introduced. Agranulocytosis associated with deferiprone has been reported.
- Deferasirox (Exjade) longer half-life in comparison with deferiprone allows this drug to be given once daily (total of 20 to 40 mg/kg/day). Side effects include gastrointestinal complaints (abdominal pain, nausea, vomiting, diarrhoea) and skin rash. There have been post marketing reports of acute renal failure, hepatic failure, and cytopenias.
Hematopoietic cell transplantation is the only curative strategy for patients with hemoglobinopathies.
- Lack of available donors is the major limitation of bone marrow transplantation.
Comments
Post a Comment