Infantile Haemangioma
Introduction
Infantile haemangioma (also known as strawberry naevus) is a common benign vascular tumour that affects up to 10% of neonates.
- It is more common in females and in premature infants.
Symptoms
The lesion may be present at birth, or appear within the first month of life.
- It may initially present as a faint pink or red patch on the skin, often mistaken for a scratch.
- The mark may then grow and evolve into the more typical prominent red lump.
Infantile haemangiomas can be
- Superficial (50-60%) - Typically has a sharp border, and is a round or oval with a smooth or slightly bump surface
- Deep (15%) - Develops under the skin and may appear as a slow-glowing skin-coloured or slightly blue lump.
- Mixed (25-35%)
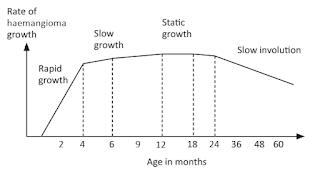
The majority of infantile haemangiomas reach their final size when the child reaches 3 months of age, but some may continue to grow until the child is 5 to 9 months old.
- The lesion then enters a slow involution phase (shrinking phase), which can take several years.
- After shrinking, larger lesions often leave excess skin, textural change and telangiectasia (visible small linear red blood vessels near the surface of the skin).
Management
Most small nonfacial haemangiomas do not need treatment.
- Can be managed with active observation and anticipatory guidance.
- For superficial lesions on the face or other areas that are cosmetically sensitive, or when treatment is desired by parents or carers, refer promptly to a dermatologist - these lesions may respond to early intervention with topical timolol and/or vascular laser therapy.
Some infantile haemangiomas require urgent medical intervention to prevent complications such as functional disturbance, severe anatomical distortion, ulceration and scarring.
- Beard - Airway compromise
- Eye - Visual obstruction, lazy eye (amblyopia), strabismus, astigmatism
- Lumbar - Tethered cord, imperforate anus, renal anomalies, sacral anomalies
- Facial - PHACES (posterior fossa structural brain abnormalities)
- Segmental haemangiomas - Associated with other congenital abnormalities
- Very large haemangiomas - Increase the risk of cardiac failure and hypothyroidism
- Large number of haemangiomas - to exclude systemic involvement
In rare circumstances, infantile haemangiomas may also become life-threatening.
Treatment
If treatment warranted,
- Topical timolol
- For smaller flat lesions.
- May also be used as adjunct to oral propranolol to delay initiation of systemic therapy or to facilitate tapering of propranolol.
- Oral propranolol
- First-line treatment for infantile haemangiomas that require systemic therapy.
- Dosing should be 2-3 mg/kg/day unless comorbidities or adverse effects require lower doses.
- Oral prednisolone
- Can be used if propranolol is contraindicated.
- Dosing: 3 mg/kg per day weaning over 6 weeks.
- Vascular laser or early surgery
- May be used in certain circumstances.
- Later in childhood after shrinking of the haemangioma has occurred, redundant skin can be removed by surgery, and residual telangiectasia and textural skin changes can be treated with laser therapy.

Comments
Post a Comment