Therapeutic Drug Monitoring (TDM)
Introduction
Theoretically, we can measure all drugs concentration in our blood. However, for the majority of medications, drug concentration monitoring is unnecessary.
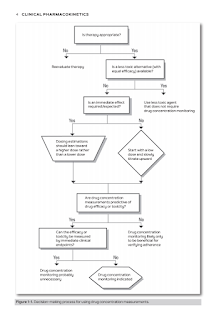
When consider using drug concentration monitoring, clinicians should ask themselves the following questions.
- Is the patient already responding appropriately to the drug therapy?
- Is the patient having any toxicity from the drug therapy?
- Is the efficacy and toxicity of this drug better predicted by measuring drug concentrations or evaluating the clinical response?
- Will obtaining a drug concentration change the clinical management of the patient?
Objectives
For simplistic purpose, there are 3 different occasions where we choose to do a TDM:
- To ensure the narrow therapeutic window drug level is within therapeutic range.
- If the drug level is found to be below or above the range, it will serve as a guide for dosage adjustment. However, the result should be interpreted in a clinical context.
- To illustrate, we will not adjust the dose of antiepileptic drug if the patient is seizure free despite has a drug level lower than therapeutic range.
- To check for drug toxicity if suspected
- E.g. Development of toxicity likely caused by a drug and liver failure due to suspected paracetamol poisoning.
- To check patient compliance to a drug
- Lack of adherence by patients to medication regimens is a frequently occurring problem.
- E.g. When a patient is suspected of not adhering to medication regimen or to rule out noncompliance issues.
Population Estimation
In TDM, we will use population pharmacokinetics developed by research to do a drug estimation.
- The population pharmacokinetic parameters can vary with ages and references.
In real practice, the estimated value may not equivalent to the actual measured value. Hence, resampling of drug is often unavoidable.
- Every one of us is uniquely different from each other, including how our body react to an administered drug.
- In other words, there could be an interpatient variability in the dose-concentration relationship or what we termed as "pharmacokinetic difference”.
- It is only after doing a TDM, we might be able to draw out a more precise estimation based on the individual patient profile.
Moreover, formulas are like our computer software, it only does that for which they are being tasked. It will be garbage in, garbage out. Hence, an appreciation should be given to the TDM formulae, instead of blindly using them.
- I have seen times that we used a wrong formula to make estimation. Consequently, a wrong estimation will be produced from the standard formula. Then, it is followed by wrong recommendations.
Sampling Time
- Randomly - To check for suspected toxicity or noncompliance
- At steady state (usually immediately pre-dose, i.e. trough concentrations taken at the end of the dose interval) - To use TDM result to dose adjustment if needed
Approximately 5 half-lives are needed to reach steady state after a drug initiation or dose adjustment, except when a loading dose is given.
- This rule is clinically significant because drugs with a short half-life will soon reach steady state concentration.
- Drugs with long half-lives or drugs that require immediate action are often given as a loading dose to take the plasma concentrations quickly up to a desired level.
Level Interpretation
When interpreting concentration measured, the following factors should be considered.
- The sampling time in relation to the dose
- Dosage history (whether or not the result represents steady state)
- Patient' response and desired clinical targets
- Missed doses
It has become a standard format in therapeutic drug monitoring recommendation in Malaysia where we will inform:
- The measured drug level, and is it subtherapeutic or in toxic range
- To withhold or continue the drug based on drug level and pharmacokinetics calculation,
- Suggest time to resample
- Recommendations on standard monitoring parameter.
Well, it is a systematic recommendation but it is never that simple and sweet.
A therapeutic range is usually used as a guide to the optimum concentration. The limits of these ranges should not be taken as absolute (i.e. Managing a patient is never based solely on therapeutic drug level. We should consider patient clinical progress too.).
- Some patients may respond to levels above or below these ranges, whereas others may experience toxic effects within the so-called therapeutic range.
- These ranges are only adjuncts to dose determination, which should always be done in the light of clinical response.
To give a justified and correct recommendation, a background knowledge on the clinical conditions that we are discussing at is much needed.
- Before discussing phenytoin drug level adjustment, we should have a basic understanding on what is meant by epilepsy and what is the first line management for each sub-type.
- Do you know that carbamazepine should not be given to manage absence seizure?
- If the drug is not indicated, the drug should not be prescribed, hence therapeutic drug monitoring would not be needed.
Useful References
For Ministry of Health settings at Malaysia, Clinical Pharmacokinetics Pharmacy Handbook is probably the most heavily used reference for therapeutic drug monitoring.
- In the 1980's, Therapeutic Drug Monitoring (TDM) service was introduced in Malaysia.
- However, only until 2015, the first edition of Clinical Pharmacokinetics Pharmacy Handbook is published to serve as standard reference for all pharmacists practicing in Ministry of Health facilities.
- 4 years later, a 2nd edition is published with few updates.
- Drugs covered include aminoglycosides, carbamazepine, cyclosporine, digoxin, lithium, methotrexate, paracetamol, phenobarbitone, phenytoin, salicylate, sirolimus, tacrolimus, valproic acid and vancomycin.
Nonetheless, there are few small errors that I come across.
- Calculation section of phenytoin at page 178.
- The equation can be used for patients receiving dialysis with low OR normal albumin level.
- Certainly, the calculated result should be used only as a guide or approximation because considerable variability has been reported.
- Calculation section of valproic acid at page 253.
- The calculated clearance is 0.85 L/hr.
- But, the clearance value used at Ke formula is 0.60.
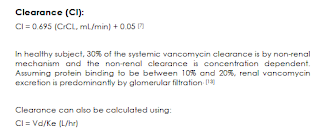
- Clearance section of vancomycin at page 257.
- The Cl and CrCl in the equation should be in the unit of ml/min/kg.
- Clearance should be Vd * Ke, instead of Vd/Ke.
Other recommended reference shall include
- ASHP Clinical Pharmacokinetics, 2021
- Applied Clinical Pharmacokinetics, 2014
- Casebook in Clinical Pharmacokinetics and Drug Dosing, 2015
- Concepts in Clinical Pharmacokinetics, 2018
- Winter's Basic Clinical Pharmacokinetics, 2023





Comments
Post a Comment