Geriatric Patients
Introduction
According to the statistics from the Department of Statistics of Malaysia, the years that babies in Malaysia in 2020 are expected to live has increased further to 74.9 years or almost 75 years. Hence, our population is actually ageing. This could be due to
- Decreased fertility
- Lower infant mortality
- Better healthcare & public health, e.g. vaccination, hygiene and nutrition
As we age, there is
- Physiological changes, for example
- Cognitive impairment, e.g. forgetful
- Reduced muscle mass and total body water
- Decreased GFR
- Deteriorating sight and hearing
- Inability to swallow solid dose form
- Loss of manual dexterity; muscle weakness
- Increased susceptibility to medical problems and complications
- Functional ability, dependence and quality of life issues are of increasing concern
- Some of the physiological changes listed above contribute to medication noncompliance.
- Serum creatinine concentration is an unreliable indicator of renal function in elderly since it may remain in the "normal" range despite a reduction in renal function due to lower muscle mass.
Polypharmacy
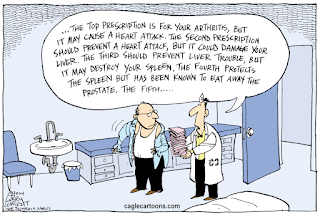
Prescribing is an art, in which we should not over-treat patients or under-treat they when they need it.
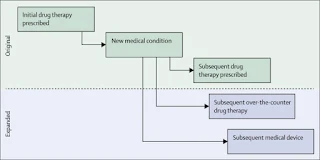
- However, as medications are the most common medical intervention, elderly patients are often expected to be on polypharmacy (i.e. regular use of >5 medications). This can lead to an increased incidence of ADRs including interactions between medications, which can then be overlooked in elderly patients and eventually lead to prescribing cascade.
In reality, polypharmacy may results from a number of factors, including
- Patients with multiple medical conditions
- Practical guidelines that recommend their use
- Fragmental systems: multiple providers (cardiologist, internist, family physician, nephrologist, etc.)
- Hospitalizations with inappropriate medication reconciliation
Despite the risks, polypharmacy is sometimes necessary as part of the optimal medical treatment. However, it is important to carefully evaluate the need for each medication and to implement only those that are truly necessary. In addition, it is important to
- Evaluate the patient's level of drug adherence
- Identify potentially inappropriate medications
- Optimize and simplify medication regimen to enhance adherence and minimise adverse effects
- Set an aim or target for the patients, such as symptom control or life prolongation
NOTE: You may find Drug-Induced Diseases, 2018 very useful in medication management review.
AGS Beers Criteria
The Beers Criteria were first developed in 1991 to decrease inappropriate prescribing and ADEs and, in particular, to identify medications or medication classes that should be avoided in older adults in nursing homes.
- Since 2011, after Beer's death, the American Geriatrics Society (AGS) began to oversee the revisions and updates to the criteria.
AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults 2023 contains six tables:
- Potentially inappropriate medication use in older adults
- Drug-disease or drug-syndrome interactions that may exacerbate the disease or syndrome
- Drugs to be used with caution in older adults
- Potentially clinically important drug-drug interactions that should be avoided in older adults
- Medications that should be avoided or have their dosage reduced with varying levels of kidney function in older adults
- Drugs with strong anticholinergic properties
Please give this important guide a read!
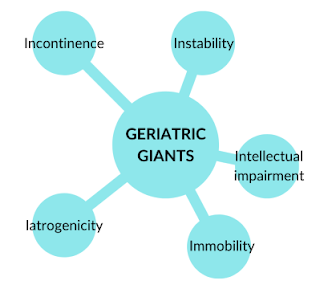
Geriatric Giants
In 1965, Bernard Isaacs coined the term "Geriatric Giants". It is often used to refer to health impairments that appear in the elderly (do not fit into any specific organ-based disease categories) and often have multifactorial causes. These health conditions may have a major impact on quality of life and disability.
You may learn more of this in Geriatric Pharmacy Pocket Book, 2021.
External Links
- AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults 2023
- Development of a Malaysian potentially inappropriate prescribing screening tool in older adults (MALPIP): a Delphi study, 2023
- Geriatric Pharmacy Pocket Book, 2021
- tl;dr pharmacy - Polypharmacy: Putting the HARM in Pharmacy, 2021
- The prescribing cascade revisited, 2017
- Facing the challenge of polypharmacy when prescribing for older people with cardiovascular disease. A review by the European Society of Cardiology Working Group on Cardiovascular Pharmacotherapy, 2022

Comments
Post a Comment