Immunization
Introduction
Immunity is acquired actively or passively.
- Active immunity develops when the person's own immune system produces antibodies to fight an infection or in response to vaccine administration.
- Lasts a long time, often a lifetime.
- Passive immunity is acquired when antibodies are provided from someone else. For example,
- Mother gives baby a copy of her immunoglobulins shortly before birth. These decrease over time as the child's own antibody production (immunity) increases.
- Intravenous immunoglobulin (IVIG) provides already made antibodies, and can be used for quick immunity after exposure to an antigen.
Immunization is one of the most effective preventive health measures.
- Vaccination programs directly benefit the immunized child. They prevent clinical manifestations or substantially reduce severity of a growing number of diseases.
- They also indirectly benefit unimmunized persons through herd immunity (such as children who are too young for immunization and persons with contraindications to vaccines.)
In layman term, vaccines work by teaching your body how to fight the germs that cause serious or deadly infections. However, unlike bacteria and viruses, they do not cause the person to fall sick to develop antibodies.
Nonetheless, in many countries, including Malaysia, adult immunisation is not commonly practiced.
Contraindications and Precautions
- Do not administer a vaccine when a contraindication is present due to an increased risk for a serious adverse reaction or anaphylactic reaction.
- Live vaccines should generally be avoided in patients that are severely immunocompromised or while the patient is taking DMARDs or biologics.
- Pregnant women should not receive live, attenuated vaccines due to theoretical risk to the foetus.
- Live virus vaccines, with the exception of yellow fever vaccine, generally should not be given during the 3 months following injection of immunoglobulin because the immune response may be inhibited.
NOTE: Examples of live vaccines include measles, mumps and rubella vaccine and the varicella (chicken pox) vaccine.
These are misconceptions about contraindications (i.e., these are not contraindications):
- Mild acute illness
- Asthma, eczema or hay fever
- Current antimicrobial therapy
- Pregnancy of the mother of the vaccine recipient
- Breastfeeding
- Allergies to antibiotics other than neomycin or streptomycin
- Food intolerances
- Family history of an adverse effect after vaccine administration
Factors Associated with Under-Immunization
- Low socioeconomic status
- Late start of vaccination series
- Missed opportunities (e.g., inappropriate contraindications above)
- Concern about potential adverse reactions
- Misconceptions that natural infection is the best way to achieve immunity.
- Belief that vaccine-preventable disease no longer poses a significant health risk
- Belief that too many vaccines all at once can overwhelm the immune system and make the child sick
- Religious or philosophical beliefs that oppose vaccinations
Adverse Events Following Immunisation (AEFI)
Most vaccines are safe and cause only mild side effects, such as
- A mild fever
- A reddish, tender area at the site of injection
- Occasionally, a "serum sickness-like" reaction that may be characterized by fever, skin rash, swollen lymph nodes, joint pain, and/or other symptoms
Very rarely, severe side effects (e.g., seizures or anaphylaxis) do occur.
The association of autism with MMR vaccination has not been proven.
- The concerns about a possible link between MMR (measles, mumps and rubella) vaccination and autism were raised by Andrew Wakefield's case series study published in The Lancet in 1998. He then recommended that the combination MMR vaccine be suspended in favour of single-antigen vaccinations given separately over time.
- The Wakefield's 1998 research received widespread attention and created the fear and distrust of all vaccines among the public.
- Only in 2004, a Sunday Times report by Deer identified his undisclosed financial conflicts of interest. Then, ten of the Wakefield's twelve co-authors of the paper later published a retraction of an interpretation.
- Till today, numerous subsequent studies cannot reproduce Wakefield's findings.
- The yellow fever and Q fever vaccines potentially contain higher amounts of egg protein and an egg allergy specialist evaluation is recommended before evaluation.
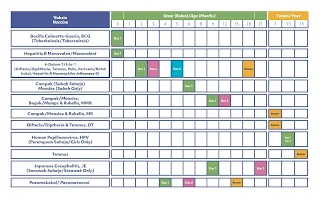
National Immunisation Programme
The Malaysian National Immunisation Programme (NIP) was introduced in the early 1950s. Our Malaysian NIP was designed based on the World Health Organisation (WHO) Expanded Programme on Immunisation. The EPI recommends that all countries immune against 6 childhood diseases, however our Malaysian National Immunisation Programme (NIP) has expanded protection against 13 major childhood disease.
Immunization During Pregnancy
There are 2 immunizations that are routinely recommended for pregnant patients.
- The inactivated influenza vaccine (NOT live) is recommended during any trimester at the beginning of flu season.
- A single dose of Tdap should be administered during each pregnancy.
Comments
Post a Comment