Breastfeeding
Introduction
Human milk is the optimal source of nutrition and protection for newborn infants because of its proven health benefits for both infants and their mothers.
- Breastfeeding is associated with child health benefits including reduced risk for acute otitis media, gastrointestinal and other infections, and may be associated with reduced risk for atopic dermatitis and asthma.
- Maternal health benefits may include reduced risk of some chronic diseases and cancer.
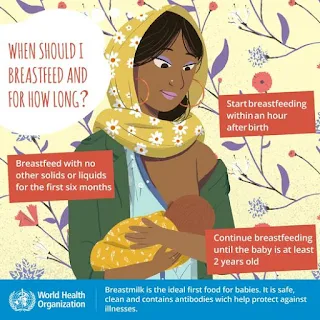
The World Health Organization recommends breastfeeding exclusively for the first 6 months of life and then continued with the addition of complementary foods for up to 2 years and beyond.
Overview of Postpartum Care
All infants should be placed skin-to-skin with the mother immediately after either vaginal or caesarean birth, unless medically contraindicated (e.g. if the mother or infant is medically unstable.
- During this period of skin-to-skin contact, a first attempt at breastfeeding should be encouraged.
- Weighing, measuring, and routine care for the infant should be delayed until the first feeding is completed.
Keeping the mother and infant together during the hospital stay has been shown to facilitate the establishment of breastfeeding and the transition to motherhood.
Decisions about medications for maternal pain management and other needs should take into account the compatibility and dosing safety with breastfeeding.
Principles of Breastfeeding
New parents should be guided to
- Expect the newborn to wake easily often to feed.
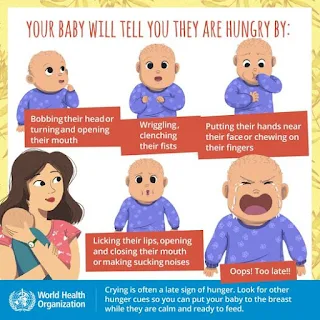
- Recognize what feeding cues in their infant look like
- Important infant cues include rooting or turning of the head, opening and closing the mouth or smacking the lips, sucking on fingers or hands.
- Feed every time the infant displays these feeding cues.
NOTE: The typical healthy newborn wakes to feed at least 8 to 12 times per 24 hours, with some variation depending on maternal and infant factors and the effectiveness of milk transfer.
The comfort of a breastfeeding position is the foundation for effective infant attachment to the breast.
An effective latch should also be clinically evaluated.
- Sucking and swallowing pattern
- Maternal nipple pain
- Shape of the mother's nipple after feeding
- Satiety cues
Milk Expression
New mothers should be taught how to express their milk using hand expression and/or a breast pump.
- Initially, this allows the mother to express milk if the infant is not feeding effectively and to stimulate her milk supply.
- Later, milk expression may be needed to relieve breast engorgement after milk production increases (lactogenesis II) or for times when the mother is separated from the infant, including returning to work.
Storage and Preparation of Breast Milk
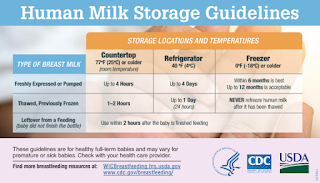
These are general guidelines for storing human milk at different temperatures.
- Various factors (milk volume, room temperature when milk is expressed, temperature fluctuations in the refrigerator and freezer, and cleanliness of the environment) can affect how long human milk can be stored safely.
- Always thaw the oldest breast milk first. Remember first in, first out.
- There are several ways to thaw your breast milk:
- In the refrigerator overnight.
- Set in a container of warm or lukewarm water.
- Under lukewarm running water.
- Never thaw or heat breast milk in a microwave. Microwaving can destroy nutrients in breast milk and create hot spots, which can burn a baby’s mouth.
Pacifier
During the first two to four weeks of life, use of a pacifier may interfere with the establishment of breastfeeding.
- Suckling on the breast is preferable because it helps to signal the mother's body to make more milk.
Once breastfeeding is well established, then the infant can be offered a pacifier for sleeping.
- Use of a pacifier during sleep appears to reduce the risk of sudden infant death syndrome (SIDS).
Infant Formula
Ideally, infant formula should be given to an infant only when there is a medical indication such as
- Clinical evidence of insufficient intake (especially excessive weight loss) or
- The mother is infected HIV or has active tuberculosis.
Feeding Bottles
Newborns typically feed every 1-3 hours, so you will need sufficient bottles (e.g., 6-8) to accommodate frequent feedings and allow for proper hygiene (including sterilization).
- As babies grow, they begin to eat more at each feeding and can go longer between feedings.
Iron
Human milk, however, is low in iron and exclusively breastfed infants will require iron supplementation.
- For full-term infants, start an iron supplement between four and six months of age (elemental iron 1 mg/kg daily, maximum 15 mg).
- Continue the supplement until the infant is taking sufficient quantities of iron-rich complementary foods (e.g., two or more servings of iron-fortified infant cereal daily).
- For premature infants, the younger the gestational age, the greater the total body iron deficit at birth.
- Start an iron supplement by two weeks of age (elemental iron 2-4 mg/kg daily, maximum 15 mg).
- Continue to provide iron at a dose of at least 2 mg/kg per day, via supplements or fortified formula, through the first year of life.
Iron deficiency anaemia is associated with anaemia and poor neurological outcomes.
Vitamin D Supplementation
Vitamin D supplementation is required for all breastfeeding infants and all formula feeding infants who are consuming <27 oz of infant formula daily.
- The recommended dose of vitamin D is 10 micrograms (400 IU) daily, beginning within few a few days after birth to prevent ricket.
Summary
Generally, babies receive all their nutrition from breast milk and/or formula for the first six months of life. Around six months, you can begin introducing solid foods, starting with small amounts of pureed foods and gradually increasing the variety and texture.
- Introducing common food allergens (like peanuts, eggs, and milk) early in a baby's diet can be safe and may help reduce the risk of those food allergies.
- Even without teeth, babies can use their gums, tongue, and palate to mash and swallow soft foods.
Signs that your baby may be ready for solid foods include:
- Sitting upright with little or no support: This indicates good head and neck control.
- Interest in food: They may watch others eat, reach for food, or open their mouths when food approaches.
- Swallowing food: They should be able to move food from a spoon into their throat without spitting it out (loss of the tongue thrust reflex). If they consistently spit food out, they may not be ready to swallow it.
NOTE: For the first six months, babies generally do not require additional water. Breast milk or formula provides adequate hydration and nutrition during this period.
External Links
- UpToDate - Initiation of Breastfeeding
- WHO - Breastfeeding
- CDC - Breast Milk Storage and Preparation
- Cleveland Clinic - Feeding Your Baby: The First Year
- Breastfeeding Your Little One
- Drugs affecting milk supply during lactation, 2018
- Early exposure to food and food allergy in children, 2014
- Early Introduction of Allergenic Foods and the Prevention of Food Allergy, 2022
Comments
Post a Comment