Iron Deficiency Anaemia
Introduction
Iron deficiency anaemia is the most common cause of anaemia worldwide, accounting for about 50% of cases.
Iron deficiency anaemia is diagnosed when iron deficiency is accompanied by anaemia.
- Low RBC, Hb, Hct, MCV,
- Decreased serum iron and increased TIBC (total iron binding capacity) resulting in a lower transferrin saturation.
NOTE: Transferrin saturation (TSAT) is the ratio of serum iron to TIBC: (serum iron ÷ TIBC x 100); if not provided directly it can be calculated. Normal values are in the range of 25 to 45%.
Dietary Iron
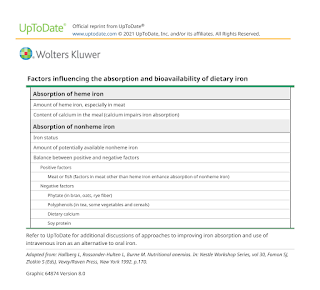
Dietary iron is available in 2 forms:
- Heme iron - found in meat and seafood
- Non-heme iron - found in nuts, beans, vegetables and fortified grains, such as cereals.
Heme iron is more readily absorbed than non-heme iron, which is affected by gastric pH and other foods being consumed, but both sources are important. Meat, seafood, poultry and ascorbic acid increase the absorption of non-heme iron, while foods that contain phytate and polyphenols (e.g. grains, beans, cereals and legumes) can decrease non-heme iron absorption. This is particularly important for patients who follow a vegetarian diet, since they are more likely to consume foods with a less absorbable form of iron along with foods that decrease the absorption of iron. Vegetarians may require iron supplementation, even if dietary intake of iron seems adequate.
Causes
- Inadequate dietary intake
- Increased need for iron (e.g. pregnancy, lactation, rapid growth during adolescence).
- Decreased iron absorption (e.g. high gastric pH, celiac disease, gastric bypass)
- Bleeding (e.g. traumatic haemorrhage, menstrual blood loss, GI haemorrhage, blood donation)
Management
Eating a diet higher in bioavailable iron can help treat iron deficiency but change in diet alone is unlikely to replete iron stores.
- Iron-rich foods include red meat, poultry, fish, beans, dark green vegetables, raisins, apricots, prunes, and iron-fortified breads and cereals.
Oral iron supplementation can adequately treat most patients with iron deficiency anaemia.
- Evidence suggests that alternate-day dosing (taking the iron every other day rather than every day) appears to result in equivalent or better iron absorption than daily dosing, usually with fewer adverse effects.
- Take oral iron on an empty stomach. If stomach upset occurs, it can be taken with food, but avoid cereals, tea, coffee, eggs, milk and high fibre products, as these decrease iron absorption.
- Vitamin C may increase the absorption of iron (by providing an acidic environment).
- Take oral iron 2 hours before or 4 hours after taking antacids.
- Iron can cause dark stools, which is expected. If you develop constipation, your healthcare provider can recommend a stool softener (e.g. docusate sodium).
NOTE: H2 antagonists and proton pump inhibitors raise gastric pH for up to 24 hours; separating the administration of these agents from iron supplements does not improve absorption.
Parenteral iron therapy is typically reserved for select patient populations due to a higher risk of side effects, cost and burden of administration.
- Indications
- Intolerance/nonadherence to oral therapy
- Chronic bleeding not manageable with oral iron
- Severe iron deficiency anaemia (Hb <8 g/dL)
- Need for rapid recovery; although the initial rise in Hb is more rapid with IV iron compared with oral iron, Hb increase at 12 weeks reported to be similar between the 2 routes.
- In patients taking erythropoiesis-stimulating agents (ESA), for example, those with anaemia of chronic kidney disease
- All parenteral iron products carry a risk of hypersensitivity reactions (including anaphylaxis).
NOTE: IV iron is contraindicated in the first trimester of pregnancy.
Patients with severe, severely symptomatic, or life-threatening anaemia should be treated with red blood cell (RBC) transfusion because correction of iron deficiency anaemia using iron replacement requires time for iron administration and incorporation into RBCs.
Follow-Up
Patients on oral iron therapy
- Initially, low hepcidin levels in patients with iron deficiency anaemia promote iron absorption resulting in rapid recovery of haemoglobin levels
- Reticulocyte count typically starts rising by 4 days after initiation of treatment and reaches maximum at 7-10 days
- Haemoglobin concentration typically increases by second week of therapy
- Optimise response to oral iron is usually defined as Hb increase of 2 g/dL after 3 weeks.
- Oral iron should be continued for 3-6 months after anaemia has been corrected in order to replenish iron stores (serum ferritin >50-100 mcg/L).
Patients on IV iron supplementation
- Ferritin should be checked every 3-4 months, and if it falls to <50 mcg/L, iron infusions should be repeated.
- Patients with continued gastrointestinal bleeding should have ferritin level checked more often and may require frequent infusions.
External Links
- DynaMed - Treatment of Iron Deficiency Anemia in Adults
- Are we giving too much iron? Low-dose iron therapy is effective in octogenarians, 2005
- Tolerability of different oral iron supplements: a systematic review, 2013
- Iron Status of Vegetarian Adults: A Review of Literature, 2016
- Systematic review and meta-analysis of iron therapy in anaemic adults without chronic kidney disease: updated and abridged Cochrane review, 2016
- Iron absorption from oral iron supplements given on consecutive versus alternate days and as single morning doses versus twice-daily split dosing in iron-depleted women: two open-label, randomised controlled trials, 2017
- Parenteral versus oral iron therapy for adults and children with chronic kidney disease, 2019
- FIP - Iron Deficiency Anemia
Comments
Post a Comment