Primary Dysmenorrhoea
Menstrual Cycle
Menstruation spans the years between menarche to menopause. Typically, this will last 30 to 40 years, starting around the age of 12 and ceasing around the age of 60.
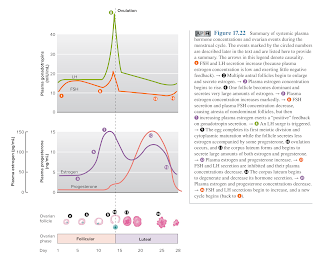
- The menstrual cycle usually lasts 28 days, but this can vary and last any time between 21 and 45 days.
- Menstruation itself lasts between 3 and 7 days.
- Individuals can also exhibit differences in menstrual cycle length and blood flow.
Symptoms
Primary dysmenorrhoea is defined as menstrual pain without organic pathology (such as endometriosis, uterine fibroids, ovarian cysts, pelvic anatomic abnormalities or infection).
- A typical presentation is of lower abdominal cramping very shortly before (6 hours) or within 24 hours of the onset of menses and rarely lasts for more than 3 days.
- Pain may radiate to lower back, groin and upper thighs.
- Commonly associated symptoms include fatigue, back pain, nausea and/or vomiting and diarrhoea.
Severe symptoms may result in school and work absenteeism and/or limitations on social, academic, and sports activities.
NOTE: There may be a gap of months or years between menarche and the onset of symptoms. This is due to as many as 50% of women being anovulatory in the first year (and still 10% of women 8 years after the menarche). This is important to know because anovulatory cycles are usually pain free.
Over-the-Counter Medication
The use of NSAIDs (e.g. ibuprofen, naproxen, mefenamic acid, celecoxib) are recommended as first-line treatment for primary dysmenorrhoea unless there is a contraindication to their use (e.g. gastrointestinal bleeding or coagulation deficiencies).
- However, there was little evidence of superiority of any individual NSAID.
- Paracetamol is an alternative treatment for patients who cannot tolerate NSAID.
Although not available OTC, oral contraceptives have been reported to be beneficial in treating primary dysmenorrhoea.
- May be considered first-line treatment for women who also desires contraception.
Scopolamine (hyoscine) butylbromide and related drugs that relax smooth muscle through muscarinic receptors can be used to treat dysmenorrhea. However, supporting data are sparse, and medication use is often limited by side effects, which typically include dry mouth, constipation, and dizziness
Nonpharmacologic Options
Good evidence supports the effectiveness of some nonpharmacologic options, including
- Exercise (including yoga)
- Vitamins, minerals and supplements
- Transcutaneous electrical nerve stimulation
- Heat therapy
- Self-acupressure
- Surgical intervention (e.g. laparoscopy, hysterectomy)
- To treat dysmenorrhea refractory to medical management
External Links
- DynaMed - Dysmenorrhea in Adults
- AFP - Dysmenorrhea, 2021
- Nonsteroidal anti-inflammatory drugs for primary dysmenorrhoea, 2003
- Improvement of primary dysmenorrhea caused by a single oral dose of vitamin D: results of a randomized, double-blind, placebo-controlled study, 2012
- Some physiotherapy treatments may relieve menstrual pain in women with primary dysmenorrhea: a systematic review, 2014
- The effects of local low-dose heat application on dysmenorrhea, 2014
- Dietary supplements for dysmenorrhoea, 2016
- Physical activity for primary dysmenorrhea: a systematic review and meta-analysis of randomized controlled trials, 2018
- Nonsteroidal antiinflammatory drug resistance in dysmenorrhea: epidemiology, causes, and treatment, 2018
- Association of tea drinking and dysmenorrhoea among reproductive-age women in Shanghai, China (2013-2015): a cross-sectional study, 2019
Comments
Post a Comment