Contraception
Introduction
The rationale of contraception is to prevent an unintended pregnancy.
- According to 2011 data, about 45% of pregnancies are unintended in the United States, with about 42% of those resulting in abortions.
NOTE: Contraception should generally be continued for 1 year after the last period if >50 years (for 2 years if <50).
Contraceptive Methods
There are many factors in selecting contraception.
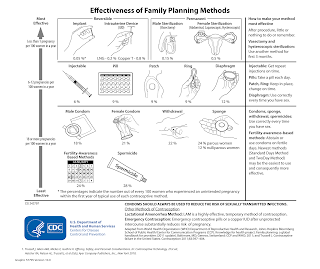
- Effectiveness
- Importance of not being pregnant
- Likelihood and ability to adhere
- Frequency of intercourse
- Age
- Cost and ability to pay
- Adverse effects
- Perceptions, misperceptions, risk-benefit
- Concomitant drug use
- Health status and habits
- Patients' preference
Women with comorbid medical conditions (e.g. thromboembolic disease, hypertension, diabetes, HIV infection, obesity, pelvic infection and seizure disorders) should be offered contraceptive methods in accordance with the WHO Medical Eligibility Criteria for Contraceptive Use or other relevant guidelines (e.g. The United States Medical Eligibility Criteria for Contraceptive Use, 2024 (US MEC)).
NOTE: Condoms should always be used to reduce the risk of sexually transmitted infections.
Postabortion
Postpartum
After a live birth, World Health Organization advises of at least 24 months before attempting the next pregnancy to reduce the risk of adverse maternal, perinatal and infant outcomes. Hence, the postpartum is an ideal timing to counsel on contraception methods.
In an overview, contraception is not necessary in the first 21 days after delivery.
Progestin-only implants and intrauterine devices (both copper and LNG-releasing IUDs) can be inserted after delivery.
Progestogen-only contraceptives may be used at any time after delivery; if depot medroxyprogesterone is used before 6 weeks postpartum, it may cause heavy, irregular heavy bleeding.
- Progestin-only pills (POPs) efficacy is likely lower than combined oral contraceptives (COC) due to the need to take them at nearly the same time every day.
- Progestogen-only contraceptives do not affect lactation.
Combined oral contraceptives (COC) is not recommended until 3 to 6 weeks postpartum as there may be increased risk of thrombosis before this time.
- The WHO Medical Eligibility Criteria for Contraceptive Use advises delaying use of oestrogen-containing methods until 6 months postpartum for women who are primarily breastfeeding.
In women <6 months postpartum who are amenorrhoeic and full breastfeeding, the lactational amenorrhoea method can be >98% effective in preventing pregnancy.
External Links
- WHO Medical eligibility criteria for contraceptive use, 2015
- The United States Medical Eligibility Criteria for Contraceptive Use, 2024 (US MEC)
- Malaysian Pharmacist Access to Contraception Education
- Effect of progestin compared with combined oral contraceptive pills on lactation: a randomized controlled trial, 2012
Comments
Post a Comment