Acne
Introduction
Acne can be defined as an inflammatory disease of the pilosebaceous follicles, causing comedones, papules and pustules on the face (99% of cases), chest (60%) and upper back (15%).
It affects approximately 80-95% of adolescents (onset typically occur at puberty).
- It usually resolves in males during their early twenties.
- Females are more likely to have ongoing acne persisting into their thirties and forties.
NOTE: Although acne is closely associated with adolescence, up to 12% of women and 3% of men aged 25 to 40 years continue to get facial acne or develop acne (late-onset acne) after adolescence.
Clinical Features
Acne lesions are classified as
- Non-inflammatory - Open (blackheads) and close (whiteheads) comedones
- Inflammatory - Pustules, red papules, nodules and cysts
- Resolving - Macules or scars
Indicative of Referral
Most cases seen in the pharmacy setting will be mild and can be managed appropriately without referral to the doctor.
- However, more persistent and severe cases (e.g. those causing significant psychological impact) need referral for more potent topical or systemic treatment.
A clinical manifestation of polycystic ovary syndrome can be acne vulgaris.
- Any woman who has menstrual irregularity (infrequent or no periods) and also exhibits hirsutism and/or is overweigh must be referred for further investigation.
General Measures
Minimise exposure to any aggravating factors.
- Drugs - e.g. anabolic steroids, some contraceptives, corticosteroids, phenytoin and fluconazole.
- In some patients, high glycaemic index foods (e.g. refined carbohydrates, sugar) and dairy products (including whey protein) can exacerbate acne severity.
- Hot, humid environments in which the face is exposed to steam, at work (e.g. chefs, baristas) or during leisure (saunas, spas) could aggravate acne.
Ensure all skincare products, cosmetics and sunscreens are noncomedogenic and nonacnegenic.
- Most "oil-free" products are noncomedogenic and less likely to aggravate acne.
- Make-up should be removed thoroughly at the end of the day.
Try not to pick and squeeze the spots, because this causes scabs that make the skin look worse.
The role of diet in acne remains poorly understood, but emerging data suggest that high glycaemic index diets (which may include sweets or chocolate) may exacerbate acne.
Treatment
For initial treatment of mild acne, suggest over-the-counter topical products (e.g. benzoyl peroxide, salicylic acid, azelaic acid and niacinamide).
- Nicotinamide is a more recent addition to the OTC market. Data suggests that it is as effective as clindamycin 1% gel; however, no randomized controlled trial seems to have been conducted to support this finding.
- One or more OTC topical products can be used for an additive effect; however this may increase irritation.
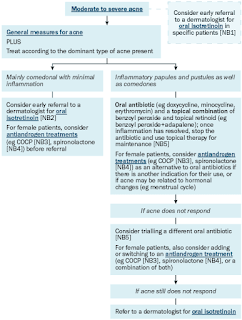
If OTC topical products are not sufficiently effective, subsequent treatment depends on the dominant type of acne present.
When treating acne, antibiotics, including topical antibiotics (e.g. clindamycin) and oral antibiotics (e.g. tetracyclines, erythromycin) are used for their anti-inflammatory action rather than their antibacterial effect.
- Avoid using antibiotics long term. Stop once papular inflammation has resolved or inflammatory acne activity is controlled.
Antiandrogens, such as combined oral contraceptive pill and spironolactone can be used to treat acne in female patients.
- Spironolactone is contraindicated in pregnancy.
NOTE: More information on benzoyl peroxide and topical tretinoin is discussed separately.
Adjunctive Therapies
Evidence of efficacy for salicylic acid and sulphur is poor. Both agents have been used for many years on the basis of their keratolytic action, but according to current evidence, they are best avoided.
Tea tree oil is a product derived from the Australian Melaleuca alternifolia tree that possesses antimicrobial and anti-inflammatory properties.- A comparative study of tea-tree oil versus benzoylperoxide in the treatment of acne, 1990
- The efficacy of 5% topical tea tree oil gel in mild to moderate acne vulgaris: a randomized, double-blind placebo-controlled study, 2007
Cosmeceuticals are intermediate products between licensed preparations containing medications and cosmetics.
- Preparations marketed for acne include those containing ceramides and retinols.
- There is insufficient evidence to support or refute their use.
Clinician-administered light sources are used for the treatment of acne, though well-designed clinical trials supporting the benefit of these treatments are limited, and there is uncertainty about the efficacy of these interventions.
Summary
While healthcare professionals may sometimes trivialize acne, it is important to remember the condition's potential for significant psychosocial effects on teenagers, including decreased self-esteem, depression, and social isolation.
- The myth that acne is caused by poor hygiene or failure to wash the skin sufficiently often is worth dispelling.
External Links
- CPG Management of Acne, 2012
- eTG Complete - Information about Acne, 2022
- Guidelines of care for the management of acne vulgaris, 2016
- Light therapies for acne, 2016
- AFP - Acne Vulgaris: Diagnosis and Treatment, 2019
- Treatment of acne with spironolactone: a retrospective review of 395 adult patients at Mayo Clinic, 2007-2017, 2020

Comments
Post a Comment