Aseptic Technique
Introduction
Aseptic technique is a skill in the compounding of sterile preparations that is independent of equipment [e.g. primary engineering control (PEC) and secondary engineering controls (i.e. cleanroom)] and environment.Proper use of Laminar Airflow Workbench (LAFW)
An LAFW should operate continuously when in use.
Before use, all interior working surfaces of the LAFW must be cleaned from the cleanest part of the LAFW to dirtiest part with sterile 70% isopropyl alcohol (IPA) or another disinfecting agent and a clean, nonshedding, lint-free wipe.
The LAFW should be cleaned and disinfected frequently, including at the beginning of the wok shift, before the start of each batch, every 30 minutes during continuous compounding periods, when there are spills, and when there is known or suspected contamination from a lapse in the aseptic technique process.
Nothing should touch the HEPA filter.
Nothing should disrupt or block the unidirectional airflow between the high-efficiency particulate (HPEA) filter and the sterile object.
Actions such as talking or coughing should be directed away from the critical area.
Only objects essential for compounding sterile preparations should be placed in the LAFW - no paper, pens, labels or trays. All items that are needed should be wiped down with sterile 70% before placing them in the LAFW.
LAFWs should be tested and certified by qualified personnel or contractors every 6 months.
Personnel Cleansing and Gowning
Remove make-up, jewellery and watch before gowning.
Don the head cover, shoe covers and face mask first because these body areas are the dirties.
Wash hands for at least 30 seconds according to the "Seven-Step Hand Washing Technique". Completely dry the hands and forearms using lint-free disposable wipes or electronic hand dryer.
After handwashing, don a nonshedding gown.
Sterile gloves must be donned as the last step and just before compounding.
NOTE: When handling hazardous drugs, wear double gloves and change the gloves every 30 minutes during hazardous drug compounding or immediately when damaged or contaminated.
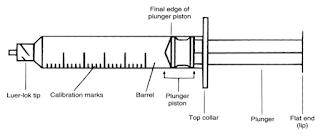
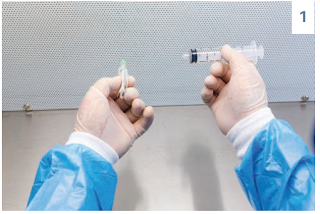
Syringes
- While opening in the LAH, open the packaging into the flow, the open plunger end of the syringe is pointing away from the compounder and toward the HEPA filter.
- While opening in the vertical flow hood, open the packaging into the flow, the open plunger end of the syringe is pointing up toward the top of the hood.
To maximize the measuring accuracy, the smallest syringe that can hold the desired amount of volume should be used; however, it should not be drawn up to the maximum capacity because the plunger could easily dislodge.
To maintain sterility, only the barrel and flat end of the syringe may be touched; the tip and the plunger cannot be touched.
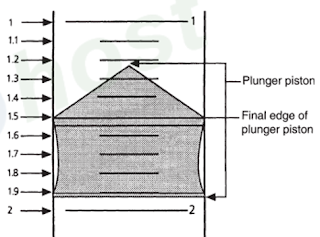
When measuring fluid in a syringe, the user should line up the final edge of plunger piston to the desired graduation mark on the barrel.
To obtain an accurate measurement, air bubbles should be removed by the following method.
- Pull back slightly on the plunger to remove any trapped fluid in the needle.
- Hold the syringe vertically with the needle pointed up and tap the syringe to force the air bubbles to the top.
- Depress the plunger to push out only the air.
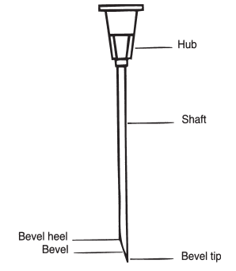
Needles
All parts of the needle are considered critical sites.
- The hub of the needle should not be touched when removing the over-wrap.
The protective cover should remain in place until the needles or syringes are used.
Used needles should not be recapped to prevent an accidental needle stick injury to the user and should be discarded into a sharp container while still attached to the syringe.
- If the needle must be recapped, it is safer to place the cap on the work surface (rather than holding it) and slip the tip of the needle into the cap, without letting the needle tip touch the work surface.
Vials
Vials are closed-system containers because air and fluid cannot pass freely in or out of them. Therefore, the volume of fluid to be removed from a vial should be replaced with an equal volume of air before withdrawing the fluid to avoid creating a vacuum.
- This technique should not be used with drugs that produce gas when reconstituted (e.g. ceftazidime) or with hazardous drugs.
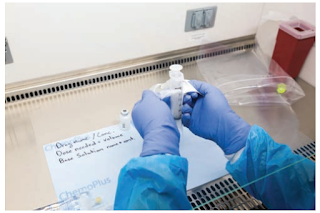
Once the vial is placed in the PEC and the cap is removed, it should be swabbed with sterile 70% IPA and allowed to dry before needle entry.
- The correct technique for swabbing the vial is several firm strokes of the swab in the same direction over the rubber stopper, using a clean, unused portion of the swab on each pass.
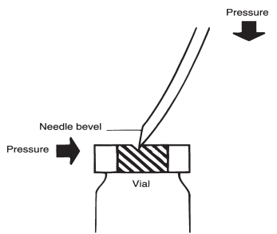
When vial stoppers are punctured with needles, there is a possibility of cores or fragments from the rubber stopper to form in the sterile liquid in the vial. To prevent this problem, the needle should be inserted in the center of the stopper at the same point with both the tip and heel of the facing up. This noncoring technique is accomplished by first piercing the rubber closure with the bevel tip and then applying lateral pressure (away from the bevel) and downward pressure to insert the needle.
Using tools such as vented needles and vented spikes will make it easier to compound when faced with negative or positive pressure.
- However, vented needles should never be used compounding hazardous drugs.
- Pressurization can be avoided by creating a slight negative pressure in the vial. Too much negative pressure, however, can cause leakage from the needle when it is withdrawn from the vial.
- The safe handling of HD solutions in vials or ampoules requires the use of a syringe that is no more than 75% full when filled with the solution. This minimizes the risk of the plunger separating from the syringe barrel.
- Once the diluent is drawn up, the needle is inserted into the vial and the plunger is pulled back (to create a slight negative pressure inside the vial) so that air is drawn into the syringe. Small amounts of diluent should be transferred slowly as equal volumes of air are removed.
- The needle should be kept in the vial, and the contents should be swirled carefully until dissolved.
- With the vial inverted, the proper amount of drug solution should be gradually withdrawn while equal volumes of air are exchanged for solution. The exact volume needed must be measured while the needle is in the vial and any excess drug should remain in the vial.
- With the vial in the upright position, a small amount of air should be drawn through the needle and just to the hub of the syringe. No additional air may be drawn into the syringe or that air will require removal prior to measuring or administering the dose. This step would create an opportunity for expelling drug or contaminated air into the environment. The hub should be clear before the needle is removed.
Ampoules
Once a glass ampoule is broken, it becomes an open system, single-user container. Because air or fluid may now pass freely in and out of them, the volume of fluid removed does not have to be replaced with air.
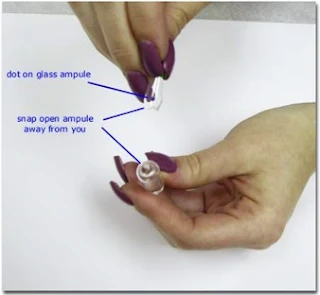
Before an ampoule is broken, any visible solution in the tap portion of head of the ampoule should be moved to the bottom or body by one of the following methods.
- Swirling the ampoule in an upright position.
- Tapping the head with one's finger
- Inverting the ampoule and then quickly swinging it into an upright position
The head of the ampoule should be held between the thumb and index finger of one hand, and the body should be held between the thumb and index finger of the other hand. Pressure should be exerted with both thumbs, pushing away from oneself in a quick motion to snap the ampoule open at the neck.
- Most ampoules are scored or have a weak point in the neck, so if ampoule does not open easily, it should be rotated so that the pressure on the neck is exerted at a different angle.
To withdraw medication from an ampule, it should be tilted and the bevel of the needle placed in the upper corner space or shoulder near the opening.
- Glass particles generally settle to the bottom of the ampule and this technique reduces the risk of aspirating glass into the syringe.
- Surface tension should keep the solution from spilling out of the tilted ampule.
- The syringe plunger is then pulled back to withdraw the solution.
The use of a sterile filter needle eliminates glass or paint chips that may have fallen into the solution from being drawn up into the syringe.
- A filter needle contains a 5-µm filter in the hub. It can be attached to the syringe before the solution is withdrawn from the ampoule or after the solution has been withdrawn.
- If it is added before withdrawing the solution from the ampoule, the filter needle must be removed after the solution is withdrawn and replaced with a new sterile needle before adding the drug to another container.
- If the solution is withdrawn from the ampoule with a regular sterile needle, that needle should be replaced with a filter needle before adding the drug to another container.
- Suspensions should be withdrawn from an ampoule using the latter technique.
- In all cases, the same filter needle should not be used for both withdrawing and injecting because it will nullify the filtering effort.
Closed System Transfer Devices
CSTDs allow the compounder to complete the hazardous drug compounding while not having to utilize a needle.
These supplemental engineering controls utilize receptacles with spikes that are placed over the rubber stoppers of vials and inserted into base solutions.
If available, these devices limit the potential for exposure of the compounder and contamination of the PEC.





An excellent and timely piece! Proper General Equipment Sterilization and Disinfection Guidelines are critical in ensuring both safety and compliance in healthcare and laboratory settings. Your insights into best practices serve as a valuable reminder of the importance of maintaining rigorous standards. Looking forward to more informative posts like this!
ReplyDeleteGreat article! In today’s high-speed packaging lines, automated inspection is becoming critical for ensuring zero-defect output. We’ve experienced this first-hand at Optomech FOSIS – Flip-Off Seal Inspection System. where we offer machine vision-based systems for inspecting caps, bottles, labels, and even silica desiccant canisters. Automation really helps in improving repeatability and audit compliance!
ReplyDelete