Glaucoma
Introduction
Glaucoma is a group of disorders characterised by a permanent loss of visual field associated with pathological cupping of the optic disc and optic nerve damage.
- It is generally linked to raised intraocular pressure, which is the main treatable risk factor, but can also occur when the intraocular pressure is within the normal range.
- Other risk factors include advancing age, family history, ethnicity, corticosteroid use, myopia, type 2 diabetes mellitus, cardiovascular disease and hypertension.
As glaucoma has no symptoms in its early stages, a complete eye exam is essential to diagnose glaucoma early.
Intraocular Pressure (IOP)
IOP is maintained by the balance between
- Production of aqueous humour by the ciliary processes and
- The outflow of aqueous humour through the trabecular meshwork and uveoscleral outflow pathway.
A test called tonometry can indirectly measure the IOP based on the pressure required to flatten a small area of the central cornea.
- Generally, an IOP of 10 to 21 mm Hg is considered normal.
- An IOP of 22 mm Hg or greater poses an increased risk of glaucoma, although one of the less prevalent forms of glaucoma is associated with a low-to-normal IOP.
Management
Open-angle glaucoma
- Occurs where drainage of the aqueous humour through the trabecular meshwork is restricted and the angle between the iris and the cornea is normal.
- Initially, this condition tends to be asymptomatic, however, as glaucoma progresses, patients may present with irreversible sight loss or visual field defects.
- Increased intraocular pressure (IOP) is its main modifiable factor.
- Initial treatment of glaucoma is generally with topical drugs; selective laser trabeculoplasty may be considered in some patients.
- Other laser or surgical interventions are considered when initial treatment is inadequate or intolerable.
Angle closure glaucoma
- Occurs when the outflow of aqueous humour from the eye is totally obstructed by bowing of the iris against the trabecular network.
- It is characterized by its abrupt onset of symptoms, and is a sight-threatening medical emergency that requires urgent reduction of IOP to prevent loss of vision.
- Initial treatment is laser iridotomy; if unsuccessful, surgical procedures are considered.
- Topical treatment may be used, particularly in those with persistent raised IOP despite laser or surgical procedures.
NOTE: Acute angle-closure crisis is an ophthalmic emergency that requires urgent referral to an ophthalmologist. Treatments used to reduce IOP prior to laser iridotomy may include a topical beta-blocker, topical alpha2 agonist, topical carbonic anhydrase inhibitor, pilocarpine, oral or IV acetazolamide or IV mannitol.
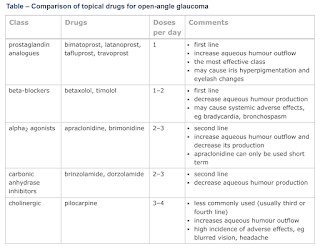
Drug Treatment for Open-Angle Glaucoma
Medical therapy is the most common initial intervention to lower intraocular pressure (IOP). Review treatment (including efficacy and adverse effects) 2-8 weeks after any change in medication and regularly thereafter.
- Prostaglandin analogues are generally first-line due to their higher efficacy, once-daily dosing and minimal systemic adverse effects.
- Prostaglandin analogues may cause iris hyperpigmentation (colour or iris appears darker) and eyelash changes. This change is permanent and may be more noticeable when only one eye is being treated.
- Topical beta-blockers are also commonly used but may cause systemic adverse effects.
- If both prostaglandin analogues and beta-blockers are not appropriate, a topical alpha2 agonist or topical carbonic anhydrase inhibitor may be used.
- Pilocarpine is less commonly used due to adverse effects.
- NO donors (e.g. Latanoprostene bunod) and ROCK inhibitors (e.g. Netarsudil) are newer agents, which can be very effective treatment options when traditional treatments have failed or are contraindicated.
If initial mediation does not achieve target IOP, consider switching medications or using a combination of medications.
- If response to a prostaglandin analogue is poor, switching to another one may be effective as drugs in this class are structurally different.
The development of fixed combination products improves adherence because of
- A reduction in the number of dosages and bottles,
- Eliminating the need to instill two separate drugs 5-10 minutes apart to prevent a washout effect from the second medication,
- Improving safety and tolerability by limiting the exposure to the BAK preservative, and
- A cost savings for the patient by potentially eliminating a copay for one of the medications.
The only oral treatment, acetazolamide, has adverse effects that limit its use to refractory glaucoma or short-term treatment pre- and post-surgery.
External Links
- American Academy of Ophthalmology - Glaucoma
- MSD Manual Professional - Glaucoma
- Meta-analysis of the efficacy and safety of alpha2-adrenergic agonists, beta-adrenergic antagonists, and topical carbonic anhydrase inhibitors with prostaglandin analogs, 2010
- Twelve-month, randomized, controlled trial of bimatoprost 0.01%, 0.0125%, and 0.03% in patients with glaucoma or ocular hypertension, 2010
- A two-year follow-up of oral antioxidant supplementation in primary open-angle glaucoma: an open-label, randomized, controlled trial, 2015
- Efficacy and safety of different regimens for primary open-angle glaucoma or ocular hypertension: a systematic review and network meta-analysis, 2018
- Efficacy and safety of prostaglandin analogues in primary open-angle glaucoma or ocular hypertension patients: A meta-analysis, 2019
Comments
Post a Comment