Red Eye
Introduction
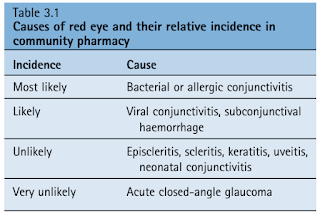
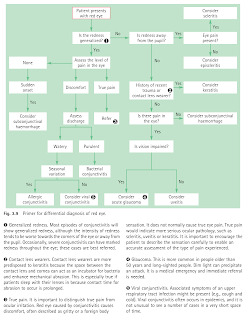
Red eye presents as both serious and non-serious eye conditions.
- Community pharmacists should differentiate manageable conditions from those requiring referral.
As a general rule, any eye condition with these symptoms requires immediate ophthalmology referral.
- Photophobia (increased light sensitivity)
- True eye pain
- Distorted vision
Conjunctivitis
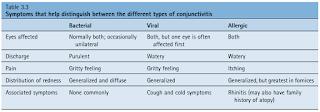
Conjunctivitis is the most common cause of red eye, characterized by varying degrees of ocular redness, irritation, itching and discharge.
Bacterial conjunctivitis is regarded as self-limiting - 65% of people will have a clinical cure in 2 to 5 days with no treatment.
- Antibiotics (e.g. chloramphenicol eye drops) are routinely given by medical practitioners (and pharmacists) to expedite recovery and decrease relapse.
No specific treatment exists for viral conjunctivitis.
Allergic Conjunctivitis
Basic eye care that are helpful to most patients with allergic conjunctivitis include
- Patient should avoid eye rubbing.
- Cold compresses can help reduce eyelid and periorbital oedema.
- Frequent use of refrigerated artificial tears throughout the day can also help to dilute and remove allergens.
- Patients should reduce or stop use of contact lenses during symptomatic periods.
Avoidance of the allergen are critical in the control of symptoms of allergic conjunctivitis.
- However, total avoidance is almost impossible.
Eye drops for allergic conjunctivitis include:
- Antihistamines (levocabastine), which provide rapid relief of symptoms.
- Mast cell stabilisers (cromoglycate, lodoxamide), which have a delayed onset (around 2 weeks) but provide longer-term relief of symptoms.
- Drugs with both antihistamine and mast cell stabilising properties (azelastine, ketotifen, olopatadine), which provide both short- and long-term relief of symptoms and appear to be more effective than drugs with only antihistamine or mast cell stabilising properties.
NOTE:
- Vasoconstrictor/antihistamine combinations (e.g. Naphcon-A) are only appropriate for short-term (e.g. less than 2 weeks) or episodic use. Regular use for longer than 2 weeks can lead to rebound hyperaemia.
- Topical NSAIDs do have efficacy compared with placebo in the treatment of allergic conjunctivitis. However, they are less effective than topical antihistamines and thus have limited utility in most cases.
Subconjunctival Haemorrhage
Although this condition is usually harmless, the appearance can be quite alarming to patients and their contacts.
- What really happened is that the blood vessels under the conjunctiva rupture, the conjunctiva cannot absorb blood very quickly, leading to subconjunctival haemorrhage.
Cause is not always known, but it can be precipitated by coughing, straining and roughly rubbing eyes.
In the absence of pain, hypertension, trauma history, or unexplained bruising/bleeding elsewhere, the patient can be reassured that symptoms should resolve spontaneously within 10 to 14 days without treatment.
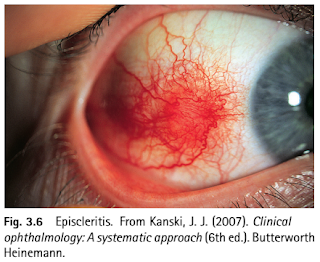
Episcleritis
The episclera lies just beneath the conjunctiva and adjacent to the sclera. If this becomes inflamed the eye appears red, which is segmental, affecting only part of the eye.
- The condition affects only one eye in the majority of cases and is usually painless; however, a dull ache might be present.
- It is more commonly seen in young women and is usually self-limiting, resolving in 2 to 3 weeks, but it can take 6 to 8 weeks before symptoms disappear.
Scleritis
Scleritis is a severe, destructive, vision-threatening inflammation.
- Of patients with scleritis, 14% lose significant visual acuity within 1 year, and 30% lose significant visual acuity within 3 years.
It is usually characterized by severe, constant, boring pain that worsens at night or in the early morning hours and radiates to the face and periorbital region.
- Additionally, patients may report headache, watering of the eyes, ocular redness, and photophobia.
Scleritis is associated with a systemic disease in approximately 50% of cases, including systemic rheumatic and inflammatory disorders, such as rheumatoid arthritis (RA) and granulomatosis with polyangiitis; and infectious diseases, including herpes zoster.
NOTE: Scleritis presents similarly to episcleritis, but pain (generally severe) is a predominant feature, as is blurred vision.
Keratitis (Corneal Ulcer)
Keratitis has generally an infectious cause (bacteria, viruses, fungi or parasites), although keratitis from other causes does occur (e.g. administration of long-term steroid drops), but is rare.
Pain, which can be very severe, is a prominent feature. The diagnostic finding in bacterial keratitis is a corneal opacity or infiltrate (typically a round white spot) in association with red eye, photophobia, and foreign body sensation.
Immediate referral is needed because loss of sight is possible if left untreated.
NOTE: Acanthamoeba infection is commonly implicated in contact lens wearers.
Uveitis
Uveitis describes inflammation involving the uveal tract (iris, ciliary body and choroids).
- The likely cause is an antigen-antibody reaction, which can occur as part of a systemic disease, such as rheumatoid arthritis or ulcerative colitis.
Photophobia and pain are prominent features, along with redness.
- The pain may be exacerbated when reading or performing close work.
- Usually, only one eye is affected, and the redness is often localized to the limbal area (known as the ciliary flush).
- On examination, the pupil will appear irregularly shaped, constricted or fixed.
Acute closed-angle glaucoma
Acute closed-angle glaucoma is relatively uncommon, but the incidence increases dramatically with age. Inadequate drainage of aqueous fluid from the anterior chamber of the eye results in a rapid increase in intraocular pressure.
- Severe unilateral eye pain associated with a headache on the same side as the painful eye is the major presenting symptom.
- The eye appears red and may be cloudy. Vision is blurred and/or decreased, and the patient might also notice haloes around lights.
- Vomiting is often experienced due to the rapid rise in intraocular pressure.
Angle-closure glaucoma is a sight-threatening emergency that must be treated within hours to avoid irreversible damage to the optic nerve.
NOTE: Diagnosis is confirmed with measurement of intraocular pressure. Normal intraocular pressure is 8 to 22 mm Hg; pressures in acute angle closure are often greater than 45 mm Hg.
External Links
- DynaMed - Red Eye - Differential Diagnosis
- UpToDate - Overview of the Red Eye
- MSD Manual Professional - Red Eye
- AFP - Diagnosis and Management of Red Eye in Primary Care, 2010
- AFP - Evaluation of the Painful Eye, 2016
- Chloramphenicol treatment for acute infective conjunctivitis in children in primary care: a randomised double-blind placebo-controlled trial, 2005
- Antibiotics versus placebo for acute bacterial conjunctivitis, 2012
- Red Alert: diagnosis and management of the acute red eye, 2014

Comments
Post a Comment