Wound Care
Introduction
Many customers walk into a pharmacy for wound care products; hence this creates opportunities for community pharmacists to be involved with simple wound management.
Wound types
- Acute wound can occur suddenly, such as burns and skin tears.
- Chronic wound is described as acute wound that have not healed after 6 weeks. It fails to progress through the normal stages of healing and can include ulcers, pressure injuries and infected wounds.
Wound Healing
Skin repair is a complex process that begins the moment a wound or injury occurs.
- The aim of skin repair is to close the wound and re-establish the skin's integrity.
- Each wound goes through the phases of cellular inflammation, destruction, proliferation and maturation.
Although the skin surface may have healed, the tissue below may still be repairing.
- It takes many months to regain full tensile strength.
NOTE: Please have a read on Describing a Wound from Presentation to Healing, 2015 to understand wound healing terminologies such as necrotic tissues, slough, granulation and epithelisation.
Moist Wound Healing
Dr George D. Winter "Formation of the Scab and the Rate of Epithelialization of Superficial Wounds in the Skin of the Young Domestic Pig" research in 1962 showed that contrary to the conventional wisdom at the time that wounds should be allowed to dry out and form scabs to promote healing, wounds instead heal faster if kept moist.
Subsequent to his early work, there has been growing, consistent evidence presented in the literature from then to the current date.
NOTE: Wound exudate has an important role in wound healing. It nourishes the tissues and flushes out foreign debris and necrotic tissue from the tissues. It is also a support medium for antibodies, enzymes and growth factors.
Wound Bed Preparation
Wound bed preparation is the systematic approach clinicians uses to identify and remove barriers to the healing process of the wound.
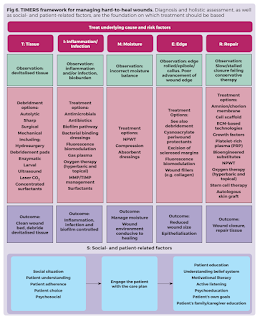
The acronym TIMERS summarises the basic principles of wound bed preparation.
- Tissue removal - Any non-viable slough or necrotic tissue must be removed if the wound is to heal.
- Infection or inflammation - Host resistance is lowered by poor nutrition and tissue perfusion, smoking, substance use, comorbidities (e.g. diabetes mellitus) and medications. If the tissue is infected, treatment with an appropriate antibiotic is required; if the tissue is inflamed, anti-inflammatory medication (e.g. steroids) should be prescribed.
- Moisture balance - A moist environment needs to be maintained, with removal of excess exudate and protection of the peri-wound from damage caused by the high level of enzymes in the exudate.
- Edge - The edge of the wound must be healthy to allow wound contraction.
- Repair or Tissue Regeneration - Some therapy includes stem cells, growth factors and oxygen.
- Social Factor - Often overlooked in chronic or slow-healing wounds.
NOTE: MEASURE framework encapsulates key wound parameters that should be addressed in the assessment and management of chronic wounds:
- Measure (length, width, depth, and area)
- Exudate (quantity and quality)
- Appearance (wound bed, including tissue type and amount)
- Suffering (pain type and level)
- Undermining (presence or absence)
- Reevaluate (monitoring of all parameters regularly)
- Edge (condition of edge and surrounding skin)
Wound Dressings
Wound dressings can be divided into two broad groups.
- Inert/passive
- Examples include gauze, lint, non-adherent dressings and tulle dressings.
- Interactive/bioactive
- Examples include semipermeable films, foams, hydroactives, alginates, hydrofibers, hydrocolloids and hydrogels.
When compared with traditional passive dressings used to cover wounds, first-line interactive dressings provide a moist, conducive environment to facilitate improved healing. These dressings are often constructed of three layers.
- The inner level prevents dressing adherence and subsequent trauma to the wound bed.
- The middle layer absorbs excess exudate and retains absorbed volume and maintains a moist environment.
- The outer layer prevents bacterial invasion.
The general rules for dressings are as follows:
- Allow 2-3 cm of dressing greater than the size of the wound.
- Place a third of the dressing above and two-thirds below the wound.
- Remove dressing when strikethrough occurs.
- Remove dressing with care in older patients.
- Do not pre-moisten alginate dressings.
- No single dressing will meet all the requirements.
Summary
Wound management is not simply applying a dressing.
- It involves an accurate diagnosis of the underlying cause and treating this cause.
- A dressing manages the wound environment, not the cause.
External Links
- MEASURE: A proposed assessment framework for developing best practice recommendations for wound assessment, 2004
- Clearing The Air About Moist Vs. Dry Wound Healing, 2014
- MOH Malaysia - Wound Care Manual, 2014
- Describing a Wound from Presentation to Healing, 2015
- The Benefits of Moist Wound Healing, 2016
- Australian Department of Veterans' Affairs - Wound Care Module, 2016
- First-Line Interactive Wound Dressing Update: A Comprehensive Review of the Evidence, 2020
- Mythbuster: ‘I need to let the air get to this wound’, 2020
- Treat the Whole of the Patient, Not the Hole in the Patient, 2020
- Wound Bed Preparation, 2021
- Wound care and dressing selection for pharmacy teams, 2021
- What Is Wound Bed Preparation?, 2022
- An update on wound management, 2023





Comments
Post a Comment