Shingles
Introduction
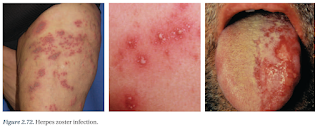
Herpes zoster (also called shingles) is a localised, blistering and painful rash caused by reactivation of varicella zoster virus.
- After primary infection of chickenpox, varicella remains dormant in dorsal root ganglia nerve cells for years before it is reactivated and migrates down sensory nerves to the skin to cause herpes zoster.
Triggering factors are sometimes recognised, such as
- Pressure on the nerve roots
- Radiotherapy at the level of the affected nerve root
- Spinal surgery
- An infection
- An injury (not necessarily to the spine)
- Contact with someone with varicella or herpes zoster
Symptoms
Herpes zoster is most often characterized by a painful, unilateral vesicular skin eruption arising in a single dermatome (or sometimes adjacent dermatomes).
- Commonly involved sites include thoracic, lumbar, cervical and trigeminal dermatomes.
- Skin eruptions are often preceded by a prodrome of pain or paraesthesias occurring 1-5 days prior to rash onset.
Patients may experience nonspecific symptoms such as headache, photophobia, and malaise but significant associated systemic symptoms such as fever are uncommon
Pain and general symptoms subside gradually as the eruption disappears.
- In uncomplicated cases, recovery is complete within 2-3 weeks in children and young adults, and within 3-4 weeks in older patients.
Complications
Post herpetic neuralgia is pain persisting for at least 3 months after shingles infection. It occurs in about 10% of all patients with shingles, and in over 70% of patients older than 50 years.
- Sometimes, instead of pain, the neuralgia results in a persistent itch (neuropathic pruritus).
Muscle weakness in about 1 in 20 patients. Facial nerve palsy is the most common result. There is a 50% chance of complete recovery but some improvement can be expected in nearly all cases.
Treatment
If the rash has been present for <72 hours, antiviral treatment (e.g. oral aciclovir, valaciclovir, famciclovir) reduces acute pain, duration of the rash, viral shedding and ocular complications.
- Whether antiviral therapy reduces the incidence of postherpetic neuralgia is contentious.
Superinfection of shingles skin lesions with Streptococcus pyogenes or Staphylococcus aureus can occur and should be treated as for impetigo or cellulitis.
- If other organisms are identified on culture, alternative antimicrobials may be required.
Manage acute pain with analgesia.
- Paracetamol or NSAIDs for mild-to-moderate pain
- Opioid analgesics, tramadol, gabapentin or pregabalin for moderate-to-severe pain.
Post-herpetic neuralgia may be difficult to treat successfully. It may respond to any of the following:
- Local anaesthetic applications (e.g. lignocaine)
- Topical capsaicin
- Tricyclic antidepressant medications (e.g. amitriptyline, nortriptyline, and imipramine)
- Anti-epileptic medications (e.g. gabapentin and pregabalin)
- Transcutaneous electrical nerve stimulation or acupuncture
- Botulinum toxin injections into the affected area.
Prevention
Because the risk of severe complications from herpes zoster is more likely in older people, those aged over 60 years might consider zoster vaccine, which can reduce the incidence of herpes zoster by half.
- In people who do get herpes zoster despite being vaccinated, the symptoms are usually less severe and post-herpetic neuralgia is less likely to develop.
External Links
- Brivudin compared with famciclovir in the treatment of herpes zoster: effects in acute disease and chronic pain in immunocompetent patients. A randomized, double-blind, multinational study, 2005
- Antivirals for management of herpes zoster including ophthalmicus: a systematic review of high-quality randomized controlled trials, 2012
Comments
Post a Comment