Antiplatelets
Introduction
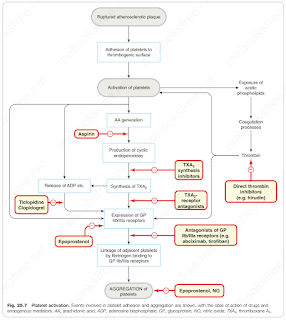
Platelets maintain the integrity of the circulation.
- When platelets are activated, they undergo a series of reactions that are essential for haemostasis, important for healing of damaged blood vessels.
Aspirin
Low-dose aspirin in chronic use profoundly (>95%) inhibits platelet TXA2 synthesis by irreversible acetylation of a serine residue in the active site of cyclo-oxygenase I (COX-1).
Owing to association with Reye's syndrome, manufacturer advises aspirin-containing preparations should not be given to children under 16 years, unless specifically indicated, e.g. for Kawasaki disease.
Contraindications to aspirin include a hypersensitivity to aspirin and major GI intolerance.
Dipyridamole
Dipyridamole inhibits platelet aggregation by several mechanisms, including
- Inhibition of phosphodiesterase,
- Block of adenosine uptake into red cells and
- Inhibition of TXA2 synthesis
It is used in addition aspirin in some patients with stroke or transient ischaemic attack.
The main side effects of dipyridamole are dizziness, headache and gastrointestinal disturbances; unlike aspirin, it does not increase the risk of bleeding.
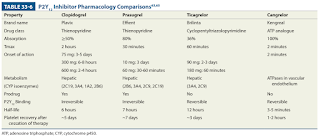
P2Y12 inhibitor
Ticlopidine was the first P2Y12 receptor inhibitor to be introduced but causes neutropenia and thrombocytopenia. The main agents are currently clopidogrel, prasugrel and ticagrelor.
In comparison to clopidogrel, prasugrel has less metabolic activation steps and a faster and more reliable onset of antiplatelet action.
- Do not use prasugrel for patients who weigh less than 60 kg, are aged 75 years or older, or who have had a previous stroke or transient ischaemic attack.
- Due to the reversible binding of ticagrelor to P2Y12 receptor, it requires twice daily dosing.
Glycoprotein IIb/IIIa inhibitors
Antagonists of the GPIIb/IIIa receptor (e.g. abciximab, eptifibatide, tirofiban) have the theoretical attraction that they inhibit all pathways of platelet activation (because these all converge on activation of GPIIb/IIIa receptors).
Besides bleeding, GP IIb/IIIa inhibitors can also cause significant thrombocytopenia in about 1% of patients receiving abciximab and 0.5% with eptifibatide and tirofiban.
The use of GP IIb/IIIa inhibitors in acute coronary syndrome has been diminished over the years.
- Although GP IIb/IIIa inhibitors have demonstrated a significant reduction in MACE in several trials, the majority of these trials were conducted before DAPT became standard of care and before the more potent P2Y12 inhibitors prasugrel and ticagrelor were available.
- In the ISAR-REACT 2 trial, patients receiving PCI for NSTE-ACS and a 600 mg loading dose of clopidogrel randomized to abciximab with heparin had a significant reduction in MACE compared to heparin alone. Interestingly, the benefit was only demonstrated in patients who had an elevated cTn (13.1% vs. 18.3%; p = 0.02), with no difference in patients without elevated cTn (4.6% in both groups).
- Hence, the patient for whom GP IIb/IIIa may provide the most benefit is one receiving PCI for NSTE-ACS with elevated cTn (e.g. suffering MI) or STEMI who has not been preloaded with P2Y12 inhibitor and is not being treated with bivalirudin.
Comments
Post a Comment