Acute Coronary Syndrome
Introduction
Acute coronary syndrome (ACS) is an acute manifestation of coronary artery disease (CAD). Patients with ACS typically experience an acute reduction in coronary blood flow most often due to a ruptured atherosclerotic plaque and subsequent formation of an intracoronary thrombus.
- The reduction in coronary blood flow produces myocardial ischemia and, if left untreated, may lead to myocardial infarction (MI).
Signs and Symptoms
The "classic" presentation of ACS is abrupt onset of substernal chest pain often described as a sensation of squeezing, heaviness, or tightness in the chest that may radiate, typically to either or both arms or shoulders (radiation to the left side is more common), the neck or the jaw. Patients with ACS may also experience diaphoresis, nausea, vomiting and dyspnoea.
As many as one-third patients may present with atypical symptoms that do not include chest pain.
- Epigastric pian
- Indigestion
- Stabbing
- Pleuritic chest pain
- Increasing exertional dyspnoea
Features that differentiate ACS from stable angina include symptom severity and duration.
- Unlike SIHD, patients with ACS often experience symptom durations lasting 10 minutes or longer.
- New or worsening symptoms of a change in symptom (e.g. acute increase in frequency or severity, occurring at rest or minimal exertion, longer duration) may be indicative of ACS.
Initial Management
The general treatment approach to ACS includes rapid diagnostic triage to determine an appropriate management strategy.
- STEMI
- Re-establishing blood flow in the occluded coronary artery (reperfusion), which is achieved with percutaneous coronary intervention or fibrinolytic therapy.
- NSTE-ACS
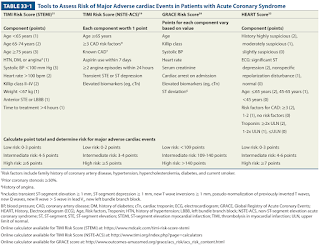
- Patients with NSTE-ACS will undergo additional risk stratification to determine the best approach, which is usually an early invasive approach (e.g., PCI) for intermediate- and high-risk patients or a more conservative, ischemia-guided management plan without planned PCI for those with either the lowest risk for coronary event or contraindications to the invasive procedure itself
- The priority for a NSTEMI is plaque stabilisation and the prevention of coronary occlusion with medical therapy, and, if appropriate, revascularisation (i.e. stenting or bypass surgery). Fibrinolytic therapy is not used to treat NSTEMI.
* Cardiac troponin is measured at the time of presentation and repeated 3 to 6 hours later to detect myocardial injury.
- There are several nonischaemic causes of myocardial injury (e.g., HF, myocarditis, Takotsubo syndrome, chronic kidney disease) that result in elevated cTn, particularly if high-sensitivity cTn assays are used. Therefore, clinical context is required to establish the diagnosis of ACS.
Chronic Management
Use of parenteral anticoagulant agents (unfractionated heparin, low-molecular-weight heparin, fondaparinux, bivalirudin) during hospitalization reduces MACE in patients with ACS.
Angiotensin-converting enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB) unless contraindicated.
Beta blocker if no contraindications.
- For at least 1 year & up to 3 years or more in patients with normal ejection fraction; indefinitely in LVEF ≤40%,
Dual antiplatelet therapy (DAPT) with aspirin plus a P2Y12 receptor inhibitor is indicated for most patients post ACS for a minimum of 12 months.
- Low-dose aspirin 75-100 mg/day will be life-long if no contraindication (e.g. hypersensitivity or major GI intolerance). If aspirin is contraindicated, consider indefinite therapy with a P2Y12 inhibitor alone.
- P2Y12 receptor inhibitor
- Ticlopidine was the first P2Y12 receptor inhibitor to be introduced but causes neutropenia and thrombocytopenia. The main agents are currently clopidogrel, prasugrel and ticagrelor.
- Do not use prasugrel for patients who weigh less than 60 kg, are aged 75 years or older, or who have had a previous stroke or transient ischaemic attack.
- Proton pump inhibitors provide a protective benefit in patients at highest risk of GI bleeding from DAPT.
Maximally tolerated statin therapy to reduce the risk of MACE, even those wtih "normal" LDL-C at baseline.
Short-acting GTN should be prescribed as needed for subsequent episode of acute angina for patients not taking phosphodiesterase-5 inhibitors.
Mineralocorticoid receptor antagonist (e.g. eplerenone, spironolactone) if the LVEF is 40% or less and either HF symptoms or diabetes mellitus are present.
Risk factor modification strategies
- Increased physical activity
- Dietary modification
- Weight loss
- Blood pressure modification
- Smoking cessation


Comments
Post a Comment