Heart Failure
Introduction
Heart failure is not a single pathological diagnosis, but a clinical syndrome consisting of cardinal symptoms (e.g. breathlessness, ankle swelling and fatigue) that may be accompanied by signs (e.g. elevated jugular venous pressure, pulmonary crackles, and peripheral oedema).
- It is due to a structural and/or functional abnormality of the heart that results in elevated intracardiac pressures and/or inadequate cardiac output at rest and/or during exercise.
- The median survival following a diagnosis is around 3 to 5 years.
A commonly used classification is by left ventricular ejection fraction (LVEF).
- HFrEF - Heart failure with reduced ventricular ejection fraction (i.e.≤ 40%)
- HFmrEF - Heart failure with mildly reduced ventricular ejection fraction (i.e. 41-49%)
- HFpEF - Heart failure with preserved ventricular ejection fraction (i.e. ≥50%)
New York Heart Association (NYHA) Functional Classification
The simplest terminology used to describe the severity of HF is the NYHA functional classification. However, this relies solely on symptoms and there are many other better prognostic indicators in HF.
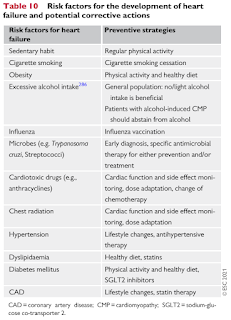
Risk Factors
Pharmacological Treatments for HFrEF Patients
Pharmacotherapy is the cornerstone of treatment for HFrEF and should be implemented before considering device therapy, and alongside non-pharmacological interventions. The 3 major goals are:
- Reduction in mortality
- Prevention of recurrent hospitalizations due to worsening HF
- Improvement in clinical status, functional capacity and quality of life
Treat all patients with HFrEF with an ACE-I (or ARB), a beta blocker and a mineralocorticoid receptor antagonist (MRA, e.g. spironolactone or eplerenone), unless contraindicated or not tolerated. Good quality clinical evidence shows that these drugs improve survival and reduce heart failure hospitalization.
- In a patients with persistent symptomatic HFrEF despite maximum doses of ACEI (or ARB), beta blocker and MRA therapies, substitution of the ACE-I (or ARB) with an ARNI may be considered; however, an ARNI can also be considered as a first-line therapy instead of an ACE-I
The sodium-glucose co-transporter 2 (SGLT2) inhibitors (e.g. dapagliflozin and empagliflozin) are recommended for all patients with HFrEF, regardless of whether they have diabetes or not, unless contraindicated or not tolerated.
- They reduced the risk of CV death and worsening HF in patients with HFrEF.
Other Drugs to be Considered in Selected Patients with HFrEF
Most symptoms and signs of heart failure are due to retention of salt and water and the consequent rise in cardiac filling pressure. Loop diuretics can be added to therapy at any stage to control congestive symptoms (e.g. breathlessness, peripheral oedema) and acute exacerbations.
- Of note, ARNI, MRAs and SGLT2 inhibitors may also possess diuretic properties.
Ivabradine can be used as an adjunct in the treatment of select patients with symptomatic HFrEF. It reduces cardiovascular death and heart failure hospitalization in patients who are in sinus rhythm, and have a heart rate of 70 beats per minute or more despite maximum tolerated dose of beta blocker therapy. Discontinue use if atrial fibrillation develops. Notable clinical trial: SHIFT.
Digoxin may be considered in patients with symptomatic HFrEF in sinus rhythm despite treatment with an ACE-I (or ARNI), a betablocker and an MRA, to reduce the risk of hospitalization (both all-cause and HF hospitalizations).
If a patient is intolerant of all three of the angiotensin system blockers (ACE-I, ARNI or an ARB), then hydralazine plus nitrate therapy (e.g. isosorbide dinitrate) can be used as an alternative (along with beta blocker therapy).
Overview of HFrEF Management
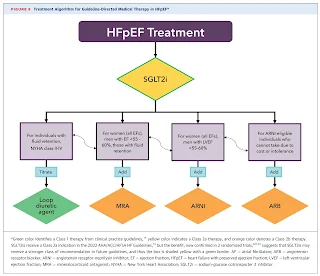
Treatment of HFpEF
To date, no treatment has been shown to convincingly reduce mortality and morbidity in patients with HFpEF, although improvements have been seen for some specific phenotypes of patients within the overall HFpEF umbrella.
- Many large RCTs conducted in HFpEF have not achieved their primary endpoints, including perindopril, candesartan, irbesartan, spironolactone, digoxin and sacubitril/valsartan.
- 2023 ACC Expert Consensus Decision Pathway on Management of Heart Failure with Preserved Ejection Fraction suggests to initiate SGLT2 inhibitors in all HFpEF patients without contraindications based on the DELIVER and EMPEROR-Preserved trials.
In the absence of recommendations regarding disease-modifying therapies, treatment should be aimed at reducing symptoms of congestion with diuretics.
- Loop diuretics are preferred, although thiazide diuretics may be useful for managing hypertension.
- Reducing body weight in obese patients and increasing exercise may further improve symptoms and exercise capacity and should therefore be considered in appropriate patients
- In general, these conditions are managed using approaches similar to those used to treat the general population or other forms of HF.
Non-Pharmacological Interventions
- Regular exercise and be physically active.
- Avoid large volume of fluid intake. A fluid restriction of 1.5-2 L/day may be considered in patients with severe HF/hyponatraemia to relieve symptoms and congestion.
- To avoid dehydration: where fluids are restricted, increase intake during periods of high heat/humidity and/or nausea/vomiting.
- Healthy diet. Avoiding excessive salt intake (>5 g/day) and maintaining a healthy body weight.
- Abstain from or avoid excessive alcohol intake.
- Immunization for influenza and pneumococcal disease
- Stop smoking (including e-cigarettes) and taking recreational drugs.
External Links
- CPG Management of Heart Failure, 2023
- ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure, 2021
- 2022 ACC/AHA/HFSA Guideline for the Management of Heart Failure
- From Primary to Tertiary Care: Expert Position Statements to Guide Heart Failure with Preserved Ejection Fraction Diagnosis, 2023
- ACC Expert Consensus Decision Pathway on Management of Heart Failure With Preserved Ejection Fraction, 2023


Comments
Post a Comment