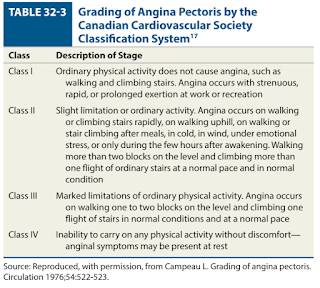
Stable Ischaemic Heart Disease
Introduction
Stable ischaemic heart disease (SIHD) is caused by obstructive atherosclerotic plaque in one or more epicardial coronary arteries.
- Inappropriate, insufficient or untreated SIHD cannot only lead to MI and cardiac death, but also cause the development of heart failure, arrhythmias and valvular disease.
Clinical Presentation
Chest pain (angina) from exertion is the cardinal symptom of myocardial ischaemia in patients with SIHD.
- In this setting, the exertion produces an increase MVO2 that exceeds what can be provided by the fixed decrease in myocardial oxygen supply from the obstructive atherosclerotic plaque.
Typically, rest or the use of sublingual nitroglycerin relieves the symptoms.
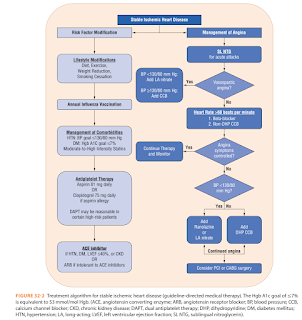
Management
The treatment of patients with SIHD typically involves 2 complementary strategies.
Slowing the progression of atherosclerosis and preventing complications such as MI, HF, stroke and death. It focuses on risk-factor modification and providing vasculoprotection therapies.
- Daily physical activity and weight management - Consider 30-60 minutes of moderate-intensity aerobic activity (such as brisk walking) at least 5 days per week.
- Dietary therapy includes reduced intake of saturated fat (to <7% of total calories), trans-fatty acids (to <1% of total calories) and cholesterol (to <200 mg/day).
- Low-dose aspirin - consider clopidogrel for aspirin allergy or intolerance cases
- Hypertension - consider ACEi or ARB
- Dyslipidaemia with maximally tolerated high-intensity statin +/- ezetimibe or PCSK-9 inhibitors
- Diabetes mellitus - consider adding SGLT2 inhibitor or GLP-1 receptor agonist to metformin
- Heart failure - consider SGLT 2 inhibitor
- Smoking cessation
- Alcohol moderation
- Annual influenza vaccination
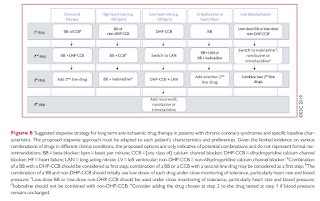
- Beta blockers and/or calcium channel blockers (e.g. verapamil and diltiazem) are typically regarded as first line therapy.
- The dose of beta blockers should be adjusted to limit the heart rate to 55-60 beats per minute at rest.
- Due to their propensity to cause reflex tachycardia, short-acting dihydropyridine calcium channel blockers (e.g. nifedipine) should be avoided when treating SIHD, chronic hypertension, hypertensive crisis or during an ACS event.
- Use of non-DHP CCBs (e.g. diltiazem and verapamil) in patients with LV dysfunction is not advised.
- Long-acting nitrates, ranolazine, trimetazidine and to a lesser extent, ivabradine, are used as additional therapy for angina.
- When long-acting nitrates are prescribed, a nitrate-free or low-nitrate interval should be considered to reduce tolerance.
- In subjects with baseline low heart rate and low BP, ranolazine and trimetazidine may be considered as first-line drug to reduce angina frequency and improve exercise intolerance.
- Trimetazidine is contraindicated in Parkinson's disease and motion disorders, such as tremor(shaking), muscle rigidity, walking disorders and restless leg syndrome.
- Sublingual and spray nitroglycerin for acute treatment.
- Spray nitroglycerin acts more rapidly than sublingual nitroglycerin.
- Nitroglycerin can be administered for prophylaxis before physical activities known to provoke angina.
- Sublingual isosorbide dinitrate has a slightly slower onset of action than nitroglycerin due to hepatic conversion to mononitrate. The effect of isosorbide dinitrate may last ≤1 h if the drug is taken sublingually or persist for several hours if the drug is taken by oral ingestion.
- Revascularization procedures may provide a survival advantage over guideline-directed medical therapy (GGDMT) in SIHD patients with more extensive atherosclerotic disease but have not demonstrated a clear advantage over GDMT in those with less extensive disease.
How to convert Isosorbide Dinitrate (Isordil) to Isosorbide Mononitrate CR (Imdex CR)? Been looking for conversion chart too
ReplyDeleteTo be honest, I have not come across a bioequivalence information on this too. However, it is probably a clinician decision when doing conversion and dose titration based on response and side effects applies too.
Delete