Intestinal Gas and Bloating
Introduction
A variety of gastrointestinal complaints, such as belching, bloating, abdominal pain and flatulence, are commonly attributed by the patient to "excess gas".
When excessive gas does occur, it may be due to
- Excessive air swallowing
- Increased intraluminal production from malabsorbed nutrients
- Decreased gas absorption due to obstruction or dysfunctional gas clearance
- Expansion of intraluminal gas due to changes in atmospheric pressure.
Differentiation of healthy individuals with temporary symptoms from those with a chronic gastrointestinal (GI) condition such as irritable bowel syndrome (IBS), lactose intolerance, or celiac disease is important in recommending appropriate nonprescription treatment.
Belching
Belching or eructation is defined as an audible escape of air from the oesophagus or the stomach into the pharynx. It may be voluntary or involuntary. Involuntary belching typically follows a meal and is caused by the release of swallowed air after gastric distention.
Belching is only considered a disorder when it is excessive and becomes troublesome.
- Individuals with belching disorder usually have habitual air swallowing (aerophagia) and air may transit only to the oesophagus before being vented (supragastric belching). In these patients, belching frequently becomes habitual and may be incorrectly regarded as being indicative of an underlying gastrointestinal disease.
- Management includes education to decrease air swallowing and reassurance that belching is a benign condition.
- Specific behavioural measures include discontinuation of gum chewing, smoking, drinking carbonated beverages, and gulping foods and liquids.
- Belching is also associated with gastroesophageal reflux disease (GERD) and functional dyspepsia. However, in patients with GERD and functional dyspepsia, belching is not the predominant symptom.
- For refractory belching: Baclofen (10 mg three times daily), by reducing transient lower esophageal sphincter relaxations and centrally suppressing the swallowing rate, may decrease both supragastric and gastric belching.
Flatulence
The volume of gas passed per rectum varies from about 500 to 1500 ml per day. The frequency of flatus released varies between 10 and 20 times per day in healthy subjects.
Although excessive passage of flatus or its foul odour may be a source of embarrassment to the patient, it is rarely associated with serious illness.
- Offensive odour, when present, may be due to sulphur-containing compounds, such as methanethiol, dimethyl sulphide, and hydrogen sulphide, as well as short-chain fatty acids, skatoles, indoles, volatile amines, and ammonia.
Management
- Treatment of the underlying cause
- Lactose restriction and the use of enzyme preparations in individuals with lactose intolerance.
- Antibiotic therapy in patients with small bowel bacterial overgrowth.
- Dietary modification
- Avoid gas-producing foods (e.g., beans, cabbage, celery, carrots, onions, broccoli, Brussel sprouts, wheat, and potatoes)
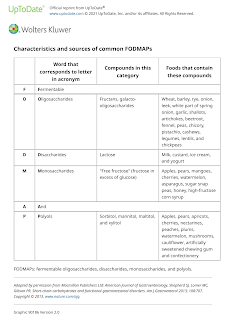
- Suggest a diet low in FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides and polyols)
- Anti-flatulence medications (e.g. simethicone and activated charcoal) and alpha galactosidase enzyme preparation
- Have not consistently demonstrated efficacy in the prevention and management of flatulence.
Abdominal Bloating and Distension
Bloating refers to a sensation of abdominal fullness, pressure, or a sensation of trapped gas, whereas distension is a measurable increase in abdominal girth.
- Other causes of abdominal girth include ascites, abdominal obesity, giant ovarian or mesenteric cyst, and bowel obstruction (mechanical or functional). These entities can typically be differentiated based on physical examination findings and if uncertain, abdominal imaging.
Management
- Treatment of the underlying cause
- Lactose restriction and the use of enzyme preparations in individuals with lactose intolerance.
- Antibiotic therapy in patients with small bowel bacterial overgrowth.
- Avoid anticholinergic agents, opioids and calcium channel blockers due to their effects on gut motility.
- Dietary modification
- Avoid gas-producing foods (e.g., beans, cabbage, celery, carrots, onions, broccoli, Brussel sprouts, wheat, and potatoes)
- Suggest a diet low in FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides and polyols)
- Restriction of carbonated drinks.
- Lifestyle modification
- Mild exercise and erect posture
- Antifoaming agents (e.g. simethicone), absorbents (e.g. activated charcoal) and probiotics
- Lacking clear evidence of efficacy in decreasing bloating/distension
Comments
Post a Comment