Venous Thromboembolism
Introduction
Venous thromboembolism (VTE) is the development of a "thrombus", principally containing fibrin and red blood cells, in the venous circulation.
- This most often occurs as a deep vein thrombosis (DVT) in the deep veins of the legs.
- If part of a thrombus breaks off and enters the right heart, it may become lodged in the pulmonary arterial circulation, causing pulmonary embolism (PE).
DVT is rarely fatal, but PE can result in death within minutes of symptom onset, before effective treatment can be given.
Risk Factors
Many risk factors fall into categories constituting what is known as Virchow’s triad: blood stasis, vascular injury and hypercoagulability.
Clinical Presentation
The symptoms of DVT or PE are nonspecific and objective tests are required to confirm or exclude the diagnosis.
- Patients with DVT frequently present with unilateral leg pain and swelling. Post thrombotic syndrome, a long-term complication of DVT caused by damage to the venous valves, may also result in chronic lower extremity swelling, pain tenderness, skin discolouration and in the most severe cases, ulceration.
- PE typically presents with chest pain, shortness of breath, tachypnoea and tachycardia, which in some cases may result in cardiopulmonary collapse.
Diagnostic Considerations
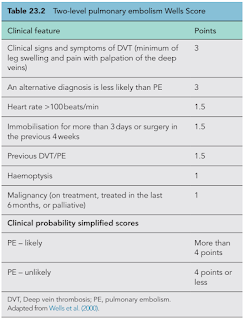
Simple clinical assessment checklists such as the Wells score can be used to determine if a patient is "likely" or "unlikely" to have DVT or PE.
Patients with an unlikely probability of VTE should first have their D-dimer tested.
- D-dimer is a fibrin clot degradation product and levels are significantly elevated in patients with acute thrombosis.
- Although D-dimer is a very sensitive marker of clot formation, it is not sufficiently specific. A variety of conditions are associated with D-dimer elevations, including recent surgery or trauma, pregnancy, advanced age, and cancer.
- However, a negative D-dimer, for most assays defined as <500 ng/mL (mcg/L), can be useful in ruling out the diagnosis of VTE.
If D-dimer above the cut-off point, the patient should have appropriate diagnostic imaging.
- Compression ultrasound (CUS) for suspected DVT
- Computed tomography pulmonary angiography (CTPA) for suspected PE
Treatment
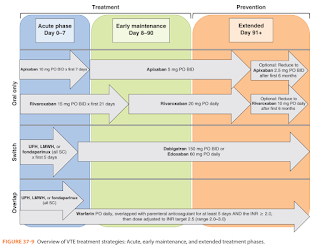
The treatment of VTE is aimed at preventing thrombus extension and embolization, reducing recurrence risk and preventing long-term complications. It involves the use of anticoagulants and, in severe cases, thrombolytic drugs.
Anticoagulation may be necessary for some time after the initial event, depending on the persistence of risk factors for recurrent thromboembolism.
- The appropriate initial duration of anticoagulation therapy to effectively treat an acute first episode of VTE for all patients is 3 months.
- To prevent new VTE episodes not directly related to the preceding episode, continuing anticoagulation therapy may be required.
- Individually tailoring anticoagulation therapy duration therapy beyond 3 months requires careful consideration of the circumstances surrounding the initial thromboembolic event, the presence of ongoing thromboembolic risk factors, bleeding risk, and patient preference.
Strict bed rest was traditionally recommended following acute DVT based on the assumption that leg movement would dislodge the clot, resulting in PE. However, ambulation in conjunction with graduated compression stockings results in faster reduction of pain and swelling with no apparent increase in embolization rate. Patients should be encouraged to ambulate as much as symptoms permit.
Prophylaxis
Effective prophylaxis can reduce the risk of fatal PE in high-risk surgical and medical populations.
- Early ambulation is often sufficient for those at low risk of VTE.
- Compression stockings and intermittent pneumatic compression (IPC) devices prevent VTE by increasing the velocity of venous blood flow through graded pressure application.
- Mechanical methods do not increase bleeding risk, which makes them attractive for postoperative VTE prophylaxis, especially in patients with contraindications to pharmacologic therapies. However, they are not risk-free, as discomfort, skin breakdown, and ulceration can occur.
- Pharmacologic options for preventing VTE (e.g. low-dose unfractionated heparin, low-molecular-weight heparin, fondaparinux, warfarin and DOACs) have been extensively evaluated in randomized clinical trials and significantly reduce the risk of VTE following hip and knee replacement, hip fracture repair, general surgery, myocardial infarction, ischemic stroke, and in selected hospitalized medical patients. The optimal agent and dose for VTE prevention must be based on an assessment of VTE and bleeding risk, as well as cost and availability.
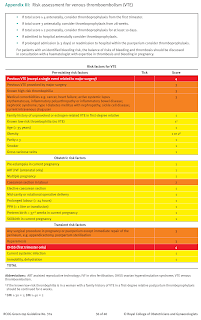
Consider VTE risk factors
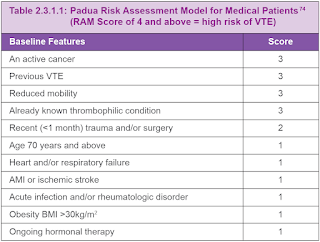
- Using Padua Prediction Score for medical patients
- Using Caprini Score for surgery patients (excludes orthopaedic surgery)
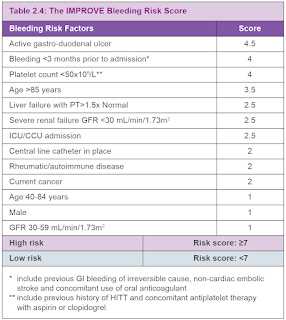
Consider bleeding risk using IMPROVE Bleeding Risk Score.
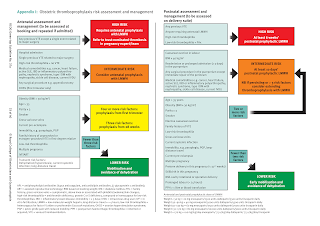
Reducing the risk of venous thromboembolism during pregnancy and the puerperium.
NOTE: Warfarin use in pregnancy is teratogenic.


Comments
Post a Comment