Chronic Kidney Disease - Mineral Bone Disorder (CKD-MBD)
Introduction
CKD mineral and bone disorder (CKD-MBD) is common in patients with renal impairment and affects almost all patients receiving dialysis.
- It is associated with fractures, cardiovascular disease and increased mortality.
Patients with advanced kidney disease require monitoring of parathyroid hormone (PTH), phosphorus, calcium and vitamin D levels.
NOTE: Renal osteodystrophy is used to describe the bone pathology asssociated with CKD.
Hyperphosphatemia
Hyperphosphatemia contributes to chronically elevated PTH levels (secondary hyperparathyroidism) and must be treated to prevent bone disease and fractures.
Treatment is initially focused on restricting dietary phosphate (e.g. dairy products, bony fish cola, chocolate and nuts).
- Dietary phosphate is restricted to 0.8-1 g/day for patients undergoing dialysis.
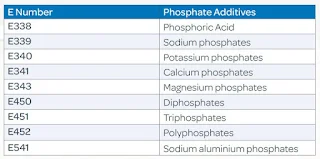
- In addition to having high phosphate content, processed foods provide a more easily absorbed form of phosphate compared with fresh animal- and plant-based foods.
- Phosphate bioavailability may be less with a vegetarian diet compared with an animal protein-based diet. Many foods that have traditionally been labeled high phosphate (such as beans and nuts) may actually be acceptable (providing they are not too high in potassium) because phosphate from these sources is absorbed slowly. This is because plant-derived phosphate found in unprocessed foods is in the form of phytate phosphorus, and the human intestine does not secrete phytase, the enzyme required for absorption. In addition, such a diet rich in legumes, nuts, and whole grains may also result in higher fiber intake while offering wider food choices
- May speak to dietitian for more practical information on phosphate counting.
As CKD progresses, phosphate binders are often required.
- Phosphate binders block the absorption of dietary phosphate.
- They are taken just prior to (or at the start of) of each meal.
- 3 types of phosphate binders
- Aluminium-based (e.g. aluminium hydroxide)
- Replaced by calcium-based phosphate binder due to aluminium toxicity.
- Calcium-based (e.g. calcium carbonate, calcium acetate)
- Calcium carbonate is first line because is cheap and effective.
- The total dose of elemental calcium provided preferably should not exceed 1500 mg/day due to risk of hypercalcemia and vascular calcification.
- Hypercalcemia is especially problematic with concomitant use of vitamin D.
- Aluminium-free, calcium-free (e.g. sevelamer, lanthanum, sucroferric oxyhydroxide, ferric citrate)
- High cost.
- Sevelamer hydrochloride, but not sevelamer carbonate, may induce metabolic acidosis.
- May be preferred in hyperphosphatemia due to reduced likelihood of positive calcium balance and hypercalcemia.
- A number of trials and two meta-analyses have suggested that non-calcium-containing phosphate binders, compared with calcium-containing phosphate binders, decrease mortality among patients with CKD.
In treatment of persistent hyperphosphatemia, dialytic phosphate removal may be employed.
Vitamin D Deficiency and Secondary Hyperparathyroidism
After controlling hyperphosphatemia, elevations in PTH are treated primarily with vitamin D.
- Vitamin D deficiency occurs when the kidney is unable to hydroxylate vitamin D to its final active.
All current vitamin D analogues may induce hyperphosphatemia and hypercalcemia, limiting the dose of which can be prescribed for CKD patients with hyperparathyroidism.
- The most commonly used vitamin D analogues are calcitriol, alfacalcidol and paricalcitol.
- Newer vitamin D analogues, such as paricalcitol and doxercalciferol, are alternatives that cause less hypercalcemia than calcitriol.
Another method of inhibiting PTH release is by increasing the sensitivity of the calcium receptor on the parathyroid gland (i.e. calcimimetic) (e.g. cinacalcet, etelcalcetide)
- Only used in dialysis patients.
- Monitor for symptoms of hypocalcaemia (e.g. paraesthesia, myalgia, cramping, tetany, seizures).
Symptomatic patients with markedly elevated parathyroid hormone (PTH) levels should be referred for parathyroid surgery if they become refractory to medical therapy.

Comments
Post a Comment