Warfarin
Introduction
Warfarin is an oral anticoagulant - a medicine that increases the time it takes for your blood to clot.
- It helps to stop unwanted clots from forming inside blood vessels. However, it does not dissolve clots, but prevents them from growing larger, allowing the body's natural system to break down the clot over time.
- A thrombosis can cause a stroke, a heart attack, a deep vein thrombosis or a pulmonary embolism.
However, warfarin use can be challenging in clinical settings due to
- Its narrow therapeutic range
- The influence of various factors on dosing such as genetic variation, drug interactions and diet.
The time spent outside the therapeutic range increases the risk of bleeding and/or thromboembolic complications that warfarin is intended to prevent.
Baseline Testing
Before initiating warfarin therapy, certain baseline tests should be obtained
- Baseline prothrombin time (PT) with international normalized ratio (INR) and baseline activated partial thromboplastin time (aPTT)
- Complete blood count (CBC) including platelet count, to obtain a baseline and identify thrombocytopenia.
- Serum creatinine, to estimate glomerular filtration rate (GFR)
- Liver function tests, to identify potential alterations of warfarin metabolism
- Urine (or serum) pregnancy test for women of childbearing potential (due to risk of teratogenicity).
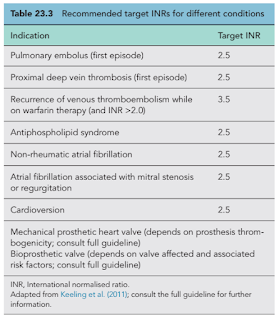
International Normalized Ratio (INR) Goals
International Normalized Ratio (INR) is a blood test that measures how long it takes for your blood to clot.
- For normal patients who are not on anticoagulation, the INR is usually 1.0.
- A higher INR means your blood is clotting more slowly and at an increased risk of bleeding.
The INR goals for warfarin therapy typically range from 2 to 3 for patients with atrial fibrillation or venous thromboembolism and somewhat higher for patients with mechanical heart valves.
- The goal of warfarin therapy is to decrease the clotting tendency of blood, but not to prevent clotting permanently. Hence, the dose of warfarin is adjusted based on the results of periodic INR tests.
- A typical frequency of INR monitoring for stable dosing is approximately every four or six weeks, assuming no changes in medications, medical condition and lifestyle.
Warfarin Dosing
Initial dosing
- An initial daily dose of ≤5 mg is suggested, unless the patient is known from previous experience to require higher doses.
- Lower starting dose (≤3 mg/day) is recommended for patients who may be sensitive to warfarin such as
- In elderly patients or in patients who are debilitated,
- Malnourished,
- Have CHF,
- Have liver disease,
- Have had recent major surgery, or
- Are taking medications known to increase the sensitivity to warfarin (e.g., amiodarone)
- Higher doses or loading dose (≥10 mg) generally do not result in more rapid therapeutic anticoagulation, but may increase the risk of supratherapeutic INR and bleeding.
- An initial effect on the INR usually occurs within the first 2-3 days [due to depletion of factor VII, but there are other vitamin K–dependent clotting factors with longer half-lives (e.g., factors II, IX, and X) which must also be depleted]. A therapeutic INR can usually be achieved within 5-10 days.
- In situations where a rapid effect is required, low-molecular-weight heparin (LMWH) should be administered concurrently with warfarin. LMWH usually can be discontinued in 5-6 days or after 2 consecutive therapeutic INR values are achieved.
INR-based Initial Dose Adjustment
- Typically, the PT with international normalized ratio (INR) is measured daily in hospitalized patients and starting on or around day 3 in healthy outpatients. Dosing on day 3 and subsequent days is based on the previous PT and INR results.
Establishing a Maintenance Dose
- Maintenance doses of warfarin vary significantly from patient to patient, ranging from <2 mg to ≥10 mg per day, and are based on PT/INR readings.
- Warfarin dosing should be calculated using weekly dosing.
- Dose can be increased or decreased up to 15% of weekly dosing.
- According to ICSI guideline, increase of 15% weekly dose would correspond to increase in INR of 1.0. Locally, for simplicity, we use 1% increase in warfarin weekly dose correspond to increase in INR of 0.1.
- The effect of dose changes may take up to 3 days to be reflected in the PT/INR.
- Thus, significant dose changes generally should be made only based on PT/INR results obtained at least 2 days after a previous dose adjustment.
Oral Administration
Clinicians often tell patients to take warfarin in the evening to allow same-day dose corrections based on INR results.
Warfarin can be taken with or without food.
If you miss a dose of warfarin, take it as soon as you remember, up to 8 hours late. If you miss it for longer, skip the missed dose and take the next dose as scheduled.
Poor INR Control
2 major factors that may lead to poor control of warfarin dosing are
- Medication adherence
- Failure to take warfarin appropriately
- Very low dietary vitamin K intake/vitamin K deficiency
- May make the patient especially sensitive to small day-to-day variations in vitamin K intake.
Drug Interactions
Patients are advised to maintain a relatively consistent level of intake rather than told to avoid vitamin K-containing foods.
- Moderate daily intake of approximately the same amount of vitamin K is likely to keep the INR more stable.
- Some foods that have a high level of vitamin K include: kale, broccoli, spinach, collard or turnip greens, lettuce, Brussels sprouts, and cabbage.
Warfarin has numerous drug interactions that may warrant a change in therapy or increased PT/INR monitoring.
- It is important to tell your doctor and pharmacist about all of the medications (including over-the-counter medications) and supplements you are taking.
Possibility of variable INR control with excessive alcohol intake or "binge" drinking.
- Limit alcohol intake to 1 to 2 servings per day.
- A serving is equal to 1 beer (12 ounces), 1 glass of wine (5 ounces) or 1.5 ounces of spirits.
Tobacco may affect warfarin efficacy, especially smokeless tobacco, which has a high vitamin K content.
Counselling and Patient Education
The major complication associated with warfarin is bleeding.
- Tell your doctor immediately if you have any unexplained bruising, bleeding, pink, red or dark brown urine, or red or black faeces.
Some common precautions to reduce the risk of bleeding
- Wear a helmet when riding a bicycle or motorcycle.
- Wear gloves when gardening.
- Shaving with an electric razor rather than a razor blade.
- Avoid using non-prescription medicines that contain a NSAID.
- Avoid sport activities which are aggressive because use of an anticoagulant is associated with an increased risk of trauma-associated bleeding.
- When seeing any health care professional, tell them you are taking warfarin.
Warfarin can also cause a rare side effect called skin necrosis or gangrene, which can cause dark red or black areas on the skin.
- This complication is more likely in people with an inherited clotting disorder called protein C deficiency, which is very rare.
- When it occurs, it is most likely to be seen during the first several days of warfarin therapy.
Warfarin is a known teratogen and is generally contraindicated during at least the first trimester of pregnancy.
Summary
For patients who prefer to avoid regular blood tests, they can discuss with their doctor whether direct oral anticoagulants (DOACs) like dabigatran, rivaroxaban, apixaban, or edoxaban might be a suitable alternative.
- Depending on individual circumstances, DOACs may not be suitable for everyone.



Comments
Post a Comment