Vitamin D Deficiency
Introduction
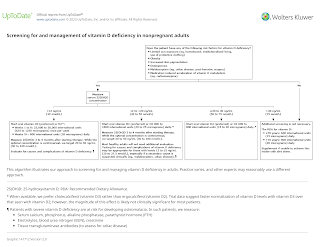
Subclinical vitamin D deficiency occurs even in developed countries and is associated with osteoporosis and possibly fractures.
- Vitamin D stores decline with age, especially in the winter.
Vitamin D Sufficiency
Vitamin D sufficiency is estimated by measuring 25-hydroxyvitamin D (25[OH]D or calcidiol) concentrations.
There are 4 main categories for the vitamin D status in individuals.
- ≥20 ng/ml (50 nmol/L): Vitamin D sufficiency
- 12 to <20 ng/ml (30-50 nmol/L): Vitamin D insufficiency
- <12 ng/ml (30 nmol/L): Vitamin D deficiency
- >100 ng/ml (>250 nmol/ml): A "risk" of vitamin D toxicity in adults ingesting substantial amounts of calcium.
According to UpToDate, the optimal serum 25(OH)D concentration for
- Maximal suppression of parathyroid hormone - >20 ng/ml (50 nmol/L)
- Adequate intestinal calcium absorption - approximately 4.4 ng/ml (11 nmol/L)
- Fracture prevention - 28 to 40 ng/ml (70 to 99 nmol/L)
Sources of Vitamin D
Sources of vitamin D include
- Sun exposure (main source)
- The best time to get sunlight is 10 am to 3 pm (midday) where the UVB rays are most intense between that period.
- Vitamin D insufficiency appears to be common among those who have increased skin pigmentation, obese or limited effective sun exposure due to protective or consistent use of sunscreens.
- Diet
- Naturally occurring food sources include fatty fish like salmon, red meat and egg yolks.
- Supplements
- Adults who do not have regular, effective sun exposure year-round should consume at least 600 to 800 IU (15 to 20 micrograms) of vitamin D3 (cholecalciferol) daily (total diet plus supplement).
- Older persons confined indoors and other high-risk groups may have low serum 25-hydroxyvitamin D (25[OH]D) concentrations at this intake level and may require higher intakes
Clinical Manifestations
The clinical manifestations of vitamin D deficiency depend upon the severity and duration of the deficiency.
The majority of patients with moderate to mild vitamin D deficiency (serum 25[OH]D between 15 to <20 ng/mL [37.5 to 50 nmol/L]) are asymptomatic. Serum calcium, phosphorus, and alkaline phosphatase are typically normal.
Patients with low vitamin D and secondary elevations in PTH are at increased risk for having accelerated bone loss, as evidenced by low bone mass on bone densitometry (dual-energy x-ray absorptiometry [DXA]) and fractures.
With prolonged, severe vitamin D deficiency, there is reduced intestinal absorption of calcium and phosphorus and hypocalcemia occurs, causing secondary hyperparathyroidism, which leads to phosphaturia, demineralization of bones, and when prolonged, osteomalacia in adults and rickets and osteomalacia in children.
Associated symptoms may then include bone pain and tenderness, muscle weakness, fracture, and difficulty walking.
Vitamin D Replacement
The amount of vitamin D required to effectively treat vitamin D deficiency depends, in part, upon the baseline level of serum 25(OH)D and also upon an individual's vitamin D absorptive capacity, capacity to convert vitamin D to 25(OH)D in the liver, and, to some extent, unknown genetic determinants.
- In patients with normal absorptive capacity, for every 100 units (2.5 mcg) of added vitamin D3, serum 25(OH)D concentrations increase by approximately 0.7 to 1.0 ng/mL (1.75 to 2.5 nmol/L), with the larger increments seen in patients with lower baseline 25(OH)D levels.
- The increment declines as the 25(OH)D concentration increases above 40 ng/mL (100 nmol/L)
External Links
- UpToDate - Vitamin D deficiency in adults: Definition, clinical manifestations, and treatment
- StatPearls - Vitamin D Deficiency
- An Update on Vitamin D Deficiency Status in Malaysia, 2022
- The impact of Vitamin D deficiency on asthma, allergic rhinitis and wheezing in children: An emerging public health problem, 2014
- An Update on the Effects of Vitamin D on the Immune System and Autoimmune Diseases, 2022
Comments
Post a Comment