Osteoporosis
Introduction
The World Health Organization (WHO) classifies low bone mineral density (BMD) according to T-score as either osteoporosis or osteopenia; these definitions only apply to BMD measurements taken at the lumbar spine, total hip or femoral neck.
- Normal = -1 or higher
- Osteopenia = Between -1 and -2.5
- Osteoporosis = -2.5 or lower
Osteoporosis occurs most commonly in postmenopausal women, men over 50 years, and in patients taking long-term oral corticosteroids (glucocorticoids).
Definitions:
- The T-Score is the number of standard deviations by which a patient's BMD varies from the young adult mean for their sex, as measured by dual energy X-ray absorptiometry (DXA).
- The Z-Score is the number of standard deviations a person's BMD varies from the age- and sex-matched mean BMD. Z-scores are recommended for reporting BMD in premenopausal women, men younger than 50 years and children.
Management
Conservative management (i.e. lifestyle changes)
- Address inadequate calcium intake and/or vitamin D deficiency
- Diet is the preferred source of calcium; only use a supplement if dietary intake is inadequate. Common calcium-rich foods include dairy products, chickpeas, beans, sardines and tofu.
- Sunlight is a source of vitamin D3 but is not ideal due to the risk of skin cancer. Dietary intake and supplements are the preferred source of vitamin D.
- Encourage patient to regularly engage in physical activity.
- Exercise throughout a person's lifetime can delay the onset of osteoporosis.
- Limiting alcohol and caffeine intake
- Smoking cessation if the patient is a current smoker
Pharmacologic therapy should be considered in people with presence or history of minimal-trauma fracture or when BMD is low (e.g. T score below -2.5, below -1.5 while on long-term corticosteroids), especially if they have other risk factors for fracture (e.g. age >70 years).
Pharmacological Treatment
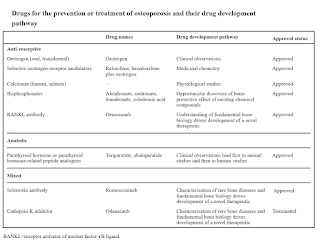
Bisphosphonates (antiresorptive medications) are first-line therapy used for prevention and treatment of osteoporosis.
- Options include alendronate (oral), ibandronic acid (oral or IV), pamidronate (IV), risedronate (oral), zoledronic acid (IV).
- Optimal duration of treatment with bisphosphonates is uncertain, but after 5 years (5 years for oral bisphosphonates, 3 years for intravenous bisphosphonates), the need for continued treatment should be assessed individually based on fracture risk.
- Bisphosphonates have been associated with the rare and serious adverse events of atypical femoral fractures and osteonecrosis of the jaw.
Alternative options include
- Denosumab
- Alternative to bisphosphonates for initial treatment
- Dosing: 60 mg single subcutaneous injection once every 6 months.
- Denosumab therapy should not be interrupted without switching to another therapy, as post-treatment bone loss can progress rapidly.
- Raloxifene
- Selective estrogen receptor modulator - NOT for male osteoporosis
- Raloxifene reduces the risk of breast cancer, but contraindicated in women with active or past history of venous thromboembolism.
- Hormonal replacement therapy
- Use is generally restricted to younger postmenopausal women with menopausal symptoms who are at high risk of fractures. This is due to the risk of adverse effects such as cardiovascular disease (e.g. stroke, VTE) and cancer in older postmenopausal women.
- Strontium ranelate, Teriparatide, Romosozumab
- Is used when other agents are unsuitable and there is a high risk of fracture.
- Strontium - 2 g granules should be stirred into at least 30 ml of water, and taken immediately at bedtime on an empty stomach; avoid food for at least 2 hours before treatment, particularly calcium-containing products, e.g. milk.
- Teriparatide - Treatment is restricted to a total of 24 months due to theoretical risk of osteosarcoma; following treatment with teriparatide, start an antiresorptive drug.
- Romosozumab - Approved for severe osteoporosis in postmenopausal women at increased risk of fractures. Do not use in patients who have had a heart attack or stroke within the previous year.
Nutritional Supplements
In addition to calcium and vitamin D supplementation, consider
Magnesium
- Several studies have investigated the effects of supplemental magnesium on bone density, generally yielding positive effects.
- In patients at risk for hypomagnesemia such as
- Patients with gastrointestinal malabsorption, renal tubular loss, or chronic liver disease (including alcohol use disorder),
- Treated with long-term diuretics or proton-pump inhibitors.
Vitamin K2 (menaquinone)
- This meta-analysis seemed to support the hypothesis that vitamin K2 plays kind of a role in the maintenance and improvement of vertebral BMD and the prevention of fractures in postmenopausal women with osteoporosis. The reduction of undercarboxylated osteocalcin and increment of osteocalcin may have some relation to the process of bone mineralization. However, the effect of vitamin K2 for postmenopausal women without osteoporosis had not been identified.
- Vitamin K deficiency results in inadequate activation of MGP, which greatly impairs the process of calcium removal and increases the risk of calcification of the blood vessels. An increased intake of vitamin K2 could be a means of lowering calcium-associated health risks.
External Links
- Treating osteoporosis: risks and management, 2022
- Osteoporosis treatment: recent developments and ongoing challenges, 2017
- Calcium beyond the bones, 2010
- Drug holidays from bisphosphonates and denosumab in postmenopausal osteoporosis: EMAS position statement, 2017
- Romosozumab Treatment in Postmenopausal Women with Osteoporosis, 2016
- Proper Calcium Use: Vitamin K2 as a Promoter of Bone and Cardiovascular Health, 2015
- Does vitamin K2 play a role in the prevention and treatment of osteoporosis for postmenopausal women: a meta-analysis of randomized controlled trials, 2015
- An update on magnesium and bone health, 2021
wow i'm glad you included raloxifene, i didnt think it is that common these days.
ReplyDelete