Antihypertensive Drugs
Introduction
For hypertension management in patients without comorbidities, recommended options in most guidelines include:
- ACE inhibitors - especially for nonblack patients and may reduce mortality
- ARBs - especially for nonblack patients but they may not reduce mortality and have limited data on comparative efficacy
- Calcium channel blockers - have limited data on mortality reduction
- Thiazide-type diuretics - shown to reduce mortality
The drug of choice for hypertension in pregnancy is still methyldopa (first line) and labetalol (alternative first line) with nifedipine as second line.
- Methyldopa, oral 250 mg TDS, doubling every 48 hours (up to 1 g TDS) until BP well controlled.
- Labetalol, oral 100 mg BD, doubling every 48 hours (up to 400 mg BD) until BP well controlled.
- Nifedipine, oral 10 mg TDS, up to 20 mg TDS, when BP poorly controlled despite maximum doses of methyldopa ± labetalol.
Beta Adrenoreceptor Antagonists
Beta-blockers are a class of drugs that slow down the heart rate and lower blood pressure. The are 2 types of beta receptors.
- β1 receptors are found mainly in the heart, where they increase the heart rate and force of contraction.
- β2 receptors are responsible for causing smooth muscle relaxation in many organs, most importantly in the lungs, where they relax the bronchioles and relieve bronchoconstriction in asthmatics.
The affinity of individual beta-blockers for beta receptors varies.
- Cardioselective (block β1 receptors)
- E.g. Atenolol, bisoprolol, celiprolol, metoprolol
- Greater affinity for β1 receptors in the heart than for β2 receptors in bronchi, peripheral vasculature and pancreas; β1-selectivity diminishes with higher doses.
- Preferred beta-blockers in COPD and well-controlled asthma, as they are less likely to precipitate bronchospasm.
- Nonselective beta blockers
- Block β1 and β2 receptors: Nadolol, pindolol, propranolol
- Block β1, β2 and α1 receptors: Carvedilol, labetalol
- Blockade of β2 receptors may cause bronchospasm.
- α1-blockade provides additional vasodilation; orthostatic hypotension is common.
NOTE: Nebivolol is β1 antagonist and β3 agonist agent.
Some beta blockers are lipid soluble and some are water soluble.
- Water-soluble beta-blockers (e.g. atenolol, celiprolol hydrochloride, nadolol and sotalol hydrochloride) are less likely to enter the brain, and may therefore cause less sleep disturbance and nightmares.
- Water-soluble beta-blockers are excreted by the kidneys and dosage reduction is often necessary in renal impairment.
Beta blockers are no longer recommended as first-line therapy in patients with uncomplicated elevated blood pressure because they are less effective than the first-line drugs in reducing the risk of stroke.
- However, they have a clear place in the management of patients with heart failure with reduced ejection fraction (HFrEF) and patients with coronary artery disease.
They should also be used with caution in people with diabetes, as they can mask the symptoms of hypoglycaemia (such as tachycardia).
Calcium Channel Blockers
Calcium channel blockers (CCBs) are a class of drugs that blocks the flow of calcium into cells. There are 3 chemically distinct classes.
- Phenylalkylamines, e.g. verapamil
- Dihydropyridines, e.g. nifedipine, amlodipine, felodipine
- Benzothiazepines, e.g. diltiazem
Verapamil preferentially affects the heart, whereas most of the dihydropyridines exert a greater on vascular smooth muscle than on the heart. Diltiazem is intermediate in its action.
Clinical uses
- Dysrhythmias: Verapamil
- Hypertension: usually a Dihydropyridine drug (e.g. amlodipine or slow-release nifedipine)
- Angina prophylaxis: a Dihydropyridine or Diltiazem
Side effects
- Short-acting dihydropyridines cause flushing and headache because of their vasodilator action, and in chronic use dihydropyridines often cause ankle swelling (oedema) related to arteriolar dilatation and increased permeability of postcapillary venules.
- Verapamil can cause constipation, probably because of effects on calcium channels in gastrointestinal nerves or smooth muscle.
- Calcium channel blockers, with the exception of amlodipine, should be avoided in heart failure as they can further depress cardiac function and exacerbate symptoms.
Diuretics
One of the key functions of the kidneys is to eliminate waste products from our body.
- The functional unit of the kidney is the nephron, and there are approximately 1400000 in each kidney (with considerable variation between individuals).
- However, nephron number declines with age, even in healthy people.
Diuretics are drugs that increase the production of urine by blocking the reabsorption of water and other substances from the kidney tubes.
- Loop diuretics (such as furosemide, bumetanide and torasemide) are the most powerful diuretics, capable of causing the excretion of 15-25% of filtered sodium.
- Thiazides (e.g. hydrochlorothiazide) and related drugs (e.g. chlortalidone, indapamide and metolazone) are diuretics acting on distal tubule. They are less powerful than loop diuretics, at least in terms of peak increase in rate of urine formation. When used in the treatment of hypertension, the initial fall in blood pressure results from the decreased blood volume caused by diuresis, but vasodilator action of thiazide diuretics contributes to the later phase.
- Aldosterone antagonists (such as spironolactone and eplerenone) and amiloride have very limited diuretic action when used singly since collecting tubule only accounts for reabsorption of only 2% of filtered sodium.
NOTE:
- Loop diuretics and thiazide diuretics may cause hypokalaemia, whereas aldosterone antagonist predispose to hyperkalaemia.
- Other drugs that can increase plasma potassium, such as ACE inhibitors, ARBs or beta antagonists, are often prescribed for patients with heart failure.
Renin-Angiotensin System
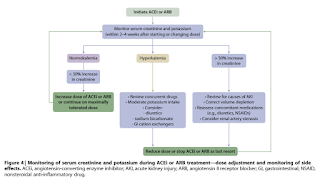
ACE inhibitor such as captopril, blocks the conversion of angiotensin I to angiotensin II. The main actions of angiotensin II are mediated via AT1 (G protein-coupled receptor).
- Generalized vasoconstriction, especially marked in efferent arterioles of the renal glomeruli;
- Increased noradrenaline release, reinforcing sympathetic effects;
- Proximal tubular reabsorption of sodium
- Secretion of aldosterone from the adrenal cortex
- Growth of cardiac and vascular cells.
NOTE: AT2 receptors are expressed during foetal life and in distinct brain regions in adults. They are believed to be involved in growth, development and exploratory behaviour.
Dry cough, possibly the result of accumulation of bradykinin, is the commonest persistent adverse effect of ACE inhibitor.
- In these cases, doctor will often switch the patients to ARBs (angiotensin II receptor antagonists).
- However, ACEIs have more robust evidence than ARBs in reducing cardiovascular morbidity and mortality (including stroke) compared with placebo in hypertension. For ethical reasons, placebo-controlled outcome data are not available for ARBs.
Frankly, these questions raised in Rang and Dale's Pharmacology made me wonder for a while.
- ACE is not the only enzyme capable of forming angiotensin II, chymase (which is not inhibited by ACEIs) providing one alternative route. It is not known if alternative pathways of angiotensin II formation are important in vivo, but if so, then ARBs could be more effective than ACEIs when such alternative pathways are active.
- Again, it is not known whether any of the beneficial effects of ACEIs are bradykinin/NO mediated. It is therefore unwise to assume that ARBs will necessarily share all the therapeutic properties of ACEIs, although there is considerable overlap in the clinical indications of these drugs.




Hi, how do we select which ACEi to be used? Some like to use Enalapril, some like to use Perindopril, I try to find comparison table but not much info (only on duration of action)
ReplyDeleteAcccording to Australian Medicines Handbook, advantages for specific ACE inhibitors are claimed based on pharmacokinetic, metabolic or tissue ACE binding characteristics, however, these do not translate into significant clinical differences. Most (except captopril) maintain an antihypertensive effect for up to 24 hours and can be given once daily.
Delete