Pain
Introduction
Pain is 'an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage'.
- In other words, it is a subjective phenomenon. Hence, if a patient finds that he is in pain, then he is in pain.
The function of acute pain is to alert the body to a potential threat, prevent the body from further damage (e.g. by moving away from the trigger), and learn to avoid similar harm in the future.
NOTE: Older people are often reluctant to disclose pain for fear of being a burden or developing a drug dependence.
Pain Assessment
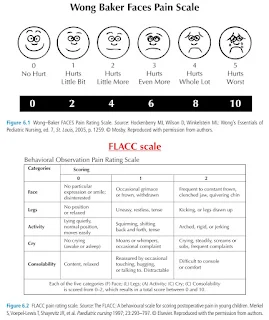
The most commonly used pain scales include
- Numerical rating scale: rates pain on a number scale, e.g. from 0 (no pain) to 10 (worst imaginable pain).
- Visual analogue scale: 10-cm-long lines labelled with an extreme at each end, usually "no pain at all" and "worst pain imaginable".
- Wong-Baker FACES Pain Rating Scale: uses pictures of faces with different expressions to rate pain.
Time-based Descriptors of Pain
Pain is best treated early because, once established, it is more difficult to treat. In addition, there is increasing evidence that appropriate early, aggressive management of acute pain may minimize the transition to chronic pain.
Acute pain
- Pain that lasts <3 months and usually has a nociceptive component.
- It can be transient and resolve quickly without the need for medical treatment (e.g. scrapes and bruises).
Recurrent pain (also referred to as episodic pain)
- Pain that occurs episodically over 3 months or more.
- Each episode is similar in presentation, e.g. inflammatory bowel disease, abdominal pain, migraine and back pain.
Chronic pain (also referred to as persistent pain)
- Pain that lasts >3 months or persisting after healing is expected to be complete.
- While it may be associated with a pathology (e.g. arthritis, cancer, spinal cord injury), often the pathology is no longer present but pain persists because of central sensitisation.
- Depression is a common comorbidity in those with chronic pain; individuals should be monitored and treated for depression as appropriate.
Pain Types
Pain may be classified clinically as
- Nociceptive
- Arises from activation of nociceptors due to actual or threatened tissue damage/
- May be somatic (e.g. involving superficial structures such as skin and muscle) or visceral (e.g. involving deeper organs such as liver, pancreas).
- Neuropathic
- Arises as a direct consequence of a lesion or disease affecting the somatosensory nervous system.
- May be peripheral (e.g. diabetic neuropathy, phantom limb) or central (spinal cord injury, post stroke) or both (postherpetic neuralgia).
- Nociplastic
- A diagnosis of exclusion
By identifying the pain type, we may optimize the pain management.
- Nociceptive pain generally responds to treatment with conventional analgesics.
- Neuropathic and nociplastic pain respond poorly to conventional analgesics and can be difficult to treat.
Nociceptive Pain
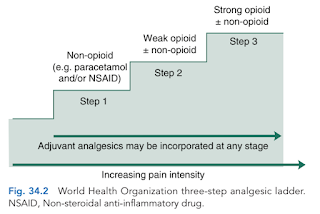
The WHO analgesic ladder is a simple approach management of nociceptive pain. Treatment starts at the step appropriate for pain severity and is adjusted according to increasing or decreasing pain severity.
- The analgesic efficacy of non-opioids, such as paracetamol, and NSAIDs, is limited by side effects and ceiling effects, that is beyond a certain dose, no further pharmacological effect is seen.
- If pain remains uncontrolled, then a weak opioid, such as tramadol, codeine or dihydrocodeine, may be helpful.
- Strong opioids, of which morphine is considered the gold standard, have no ceiling effect, and therefore increased dosage continues to give increased analgesia, but side effects often limit the effectiveness.
- Adjuvant drugs, such as corticosteroids, antidepressants or antiepileptics, may be utilised at any step of the ladder.
Neuropathic Pain
TCAs (e.g. amitriptyline, nortriptyline) and antiepileptics (e.g. carbamazepine, gabapentin, pregabalin) are considered the drug treatment of choice.
- Comparative studies are limited and provide no evidence of clinical superiority for an individual drug.
- Patients who fail to response to one drug may respond to another (even with the same drug class).
- Using drugs from 2 different classes may be more effective than either drug alone.
Of all antidepressants, duloxetine (a serotonin noradrenaline reuptake inhibitors) has the largest evidence base to support analgesic efficacy, and is effective and FDA approved for the treatment of painful diabetic neuropathy, fibromyalgia, chronic low back pain, and osteoarthritis.
- In addition to these indications, duloxetine is approved by the FDA for treatment of major depression, anxiety, and stress urinary incontinence.
Non-Drug Treatment
This includes cognitive behavioural therapies, heat or cold applications, massage, exercise, immobilisation, transcutaneous electrical nerve stimulation (TENS).
- Cognitive behavioural therapies, relaxation techniques and massage are beneficial in chronic pain, but evidence for their efficacy and that of other non-drug methods in acute pain is inconclusive.
Surgery and invasive procedures including neural blockade or spinal cord stimulation are other options.
tnx for this post
ReplyDelete