Schizophrenia
Introduction
Schizophrenia is a major psychiatric disorder that alters an individual's perception, thought, affect and behaviour.
- Onset is usually between adolescence and early adulthood.
- Most patients fluctuate between acute episodes and remission. Residual symptoms may present between episodes.
Risk Factors
Family history of schizophrenia.
Substance-induced psychoses associated with cannabis, hallucinogens and amphetamines.
Increasing paternal age.
Most urban environment.
Refugee and migrant status.
History of obstetric complications, e.g. pre-eclampsia and extreme prematurity.
Prenatal exposure to infections, e.g. Herpes Simplex (HSV-2) and toxoplasma gondii.
History of childhood central nervous system infection.
Symptoms
The Diagnostic and Statistical Manual for Mental Disorders (DSM-5) identifies 5 symptoms for diagnosis.
- At least 2 of the following symptoms must be present for at least 1 month, and
- Delusions
- Hallucinations
- Disorganized speech (e.g. frequent derailment or incoherence)
- Grossly disorganized or catatonic behaviour
- Negative symptoms (i.e. diminished emotional expression or avolition)
- At least 1 the symptoms should be delusions, hallucinations or disorganized speech.
- Continuous signs of disturbance must be present for at least 6 months.
NOTE: Hallucinations are the sensations that occur even without any external stimuli, involving hearing, seeing, smelling, tasting or feeling things that are not really there. Delusions are fixed false beliefs that the person thinks are real.
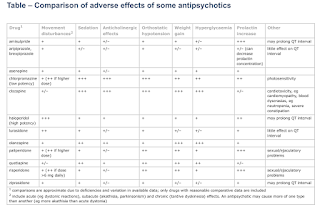
Antipsychotics
Antipsychotics provide effective protection against relapse, at least in the short to medium term.
- They are thought to be mediated (at least in part) by blockade of dopaminergic transmission (D2 receptors) in various parts of the brain (in particular the limbic system).
Relative liability for inducing EPS (extrapyramidal syndrome) was originally the primary factor behind the typical and atypical classification.
- Of these medications, perhaps only clozapine and quetiapine are "fully" atypical, seemingly having a very low liability for EPS.
- Other show dose-related effects, although, unlike with typical drugs, therapeutic activity can usually be achieved without EPS.
Hence, typicals and atypicals were reclassified as first- or second-generation antipsychotics.
- As a class, SGAs may have a lower propensity to cause EPS and tardive dyskinesia, but this is somewhat offset by a higher propensity to cause metabolic adverse effects (e.g. increased blood glucose, weight gain and dyslipidaemia).
General Principles of Prescribing
For most patients, the use of a single antipsychotic (with or without additional mood stabiliser or sedatives) is recommended.
- There is no definitive evidence that one antipsychotic is superior to another, with possible exception of clozapine.
- The choice of a particular antipsychotic agent will typically occur in the context of discussion with the patient about the likely benefits and possible side effects of medication options and will incorporate patient preferences; the patient's past responses to treatment (including symptom response and tolerability); the medication's side-effect profile; the presence of physical health conditions that may be affected by medication side effects; and other medication-related factors such as available formulations, potential for drug-drug interactions, receptor binding profiles, and pharmacokinetic considerations
- Combinations of antipsychotics should only be used where response to a single antipsychotic (including clozapine) has been clearly demonstrated to be inadequate.
The lowest possible dose should be used.
- For each patient, the dose should be titrated slowly to the lowest known to be effective.
- There is no firm evidence that high doses of antipsychotic medication are any more effective than standard doses for schizophrenia. This holds true for the use of antipsychotic medication for rapid tranquillisation, relapse prevention, persistent aggression and management of acute psychotic episodes.
- High-dose antipsychotic treatment is clearly associated with a greater side-effect burden.
- Severe neutropenia due to agranulocytosis (Absolute Neutrophil Count <500 cells/mm3) is the most limiting adverse effect.
Long-term treatment is generally required to prevent relapses.
- Antipsychotics should never be stopped abruptly.
Electroconvulsive Therapy (ECT)
Electroconvulsive therapy (ECT) may be a useful adjunct to antipsychotic when there is a need for rapid improvement and reduction in symptoms or limited response to antipsychotics in schizophrenia.
- ECT is also indicated for major psychiatric illness including major depression and mania (including bipolar disorder).

Comments
Post a Comment