Medication History Taking and Medication Reconciliation
Introduction
When a patient is admitted to Emergency Department or wards, the admitting doctor will perform a quick history taking of patient including their medication. Hence, why is there still a need for pharmacists to perform another medication history taking?
- This is because studies have shown that pharmacist-recorded medication histories result in higher accuracy and fewer medication errors.
In other words, medication history taking by pharmacists helps to retrieve missing information with regard to prescription medications which the patient is currently on, information on past drug history as well as self-medication.
Performing Medication History Taking
Ideally, CP1 form should be filled within the first 24 hours after patient admission.
In performing a medication drug history taking,
- Ideally, use a source of information that is different from the admission history.
- GP's referral letter or computer printout
- Copy of repeat prescription
- Medications that they brought in from home
- Talk to the patient/relative/carer
- Residential home medication administration record (MAR) chart
- A deep conversation with patient might reveals
- Drugs that might otherwise be overlooked (e.g. oral contraceptive pill, regular OTC medicines or herbal medicines).
- Any discrepancies between what has been prescribed and what the patient normally takes (i.e. intentional or non-intentional compliance).
- Any problems with or questions about their medication (e.g. possible drug-related problems).
- Compliance assessment can be done using Malaysia Medication Adherence Assessment Tool (MyMAAT).
Medication Reconciliation
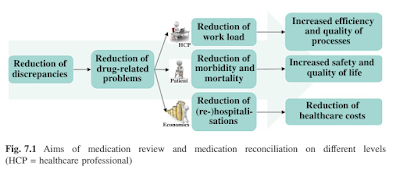
Medication reconciliation is a systematic process where all medications are correctly and consciously continued, discontinued or modified in a timely manner at each point in which the patient moves through the various levels of the healthcare continuum (e.g. after patient admission to wards).
There are 2 stages to medication reconciliation.
- Stage 1: Identification of a patient's existing medication list (prior to hospital admission) (i.e. filling up CP1 form)
- Stage 2: Comparison of the medication endorsed in the ward to the existing medication list on CP1 form, and acting upon discrepancies, unless there is a good reason to omit them.
As part of medication reconciliation, it is vital that any allergies are established along with the nature of the reaction.
Applications at Daily Work
Ideally, the CP1 form (medication history assessment form) filled should be used at 3 occasions to provide a thorough patient care.
- Initial admission
- Transfer of patients to other wards (transition of care)
- Patient discharge
In the transition of care, omission of drugs could occur. Hence, at these stages, clinical pharmacist should actively re-perform medication reconciliation to minimize the potential errors.
On the other hand, at the time of patient discharging to home, clinical pharmacists should compare the discharge medication prescription with the initial medication history assessment form. By doing this, we can identify any medication changes that we should notify the patients and give a proper counselling for those newly started medications.

Comments
Post a Comment