Systemic Lupus Erythematosus
Introduction
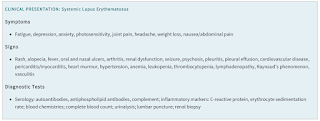
Systemic lupus erythematosus (SLE or commonly referred to as lupus) is an autoimmune disease associated with autoantibody production, primarily affects young women, with a female-to-male ratio of 10:1.
- The disease predominantly occurs in people age 15-45 years and it is more common in women of African-American and Asian descent.
Symptoms
Systemic lupus erythematosus can involve almost any organ and may present in different ways.
- Fatigue is common, but does not help distinguish SLE from other diseases.
- Arthritis and cutaneous manifestations [e.g. malar rash ("butterfly rash") and photosensitivity] are most common, but renal, hematologic and neurologic manifestations contribute largely to morbidity and mortality.
Triggering Factors
Factors such as sunlight, certain drugs and viral infection are known to trigger SLE, but the underlying cause is not fully understood.
Drugs that include lupus include
- Methimazole
- Propylthiouracil
- Methyldopa
- Minocycline
- Procainamide
- Hydralazine
- Anti-TNF agents
- Terbinafine
- Isoniazid
- Quinidine
NOTE: Drug-induced lupus erythematosus (DILE) usually resolves within weeks after drug discontinuation.
Management
Ideally, the goal should be remission, but complete remission with the absence of clinical activity and no use of glucocorticoids or immunosuppressive therapy is rare.
- Mild symptoms can be managed with NSAIDs with or without other analgesics.
- Hydroxychloroquine
- is recommended for all patients with SLE and is the cornerstone of therapy.
- Due to the risk of retinal toxicity, most patients should not receive a daily dose >5 mg/kg/day using actual body weight or 400 mg, whichever is lower.
- Corticosteroids
- Are used to most forms of SLE and up to 57-86% of patients receive continuous or chronic therapy.
- Chronic use of any dose is associated with cardiovascular complications, psychological disturbances, glaucoma, cataracts, hyperglycaemia, weight gain, avascular necrosis of bone, and osteoporosis.
- Hence, if glucocorticoid use is required, treatment should be minimized and tapered as soon as possible. Moreover, initiation of immunomodulatory agents may also aid in tapering.
- In patients who are not responding to hydroxychloroquine (alone or in combination with glucocorticoids) or patients who are unable to reduce oral prednisolone dose (or equivalent) ≤7.5 mg/day, consider the addition of
- Immunosuppressive agents, such as methotrexate, azathioprine, mycophenolate mofetil, cyclophosphamide.
- Biologics, such as anifrolumab, belimumab, rituximab.
Lifestyle modifications
- Rest and proper exercise to manage the fatigue.
- Weight control.
- Smoking cessation is encouraged since tobacco smoke can exacerbate SLE and diminish the effectiveness of antimalarials and belimumab.
- Since photosensitivity is common in SLE, sunscreens and sun protection/avoidance are recommended.

Comments
Post a Comment