Chronic Kidney Disease
Introduction
The kidneys are responsible for the following functions:
- Regulation of fluid volume, osmolarity, blood pressure, electrolyte concentrations and acidity
- Excretion of metabolic end products and foreign substances such as urea, toxins and drugs
- Synthesis of renin, erythropoietin and calcitriol
Assessing kidney function is an important skill not only for determining the appropriateness of drug dosages but to help with ongoing monitoring and management of kidney disease.
NOTE: While creatinine is commonly utilized, it is not perfect as creatinine is a metabolic by-product of muscle catabolism, meaning patients with lower or higher than average muscle will demonstrate different values than expected based on their renal function. Medications including cimetidine and trimethoprim can also impact the secretion of creatinine in the proximal tubule.
Definition
CKD is defined by the presence of kidney damage or decreased kidney function for 3 or more months, irrespective of the cause.
- It is a state of progressive loss of kidney function, ultimately resulting in the need for renal replacement therapy (dialysis or transplantation).
NOTE: The term "end-stage kidney disease" (ESKD) generally refers to chronic kidney failure treated with either dialysis or transplantation.
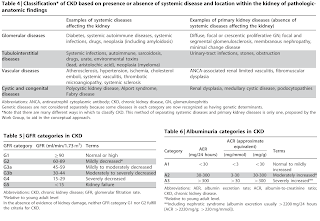
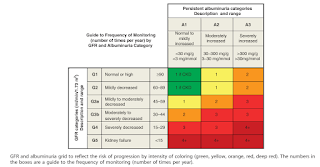
CKD Staging
Staging of CKD is done according to
- Cause of disease
- 6 categories of GFR (G stages)
- 3 categories of albuminuria (A stages)
The purpose of CKD staging is to guide management, including stratification of risk for progression and complications of CKD.
- Risk stratification is used to inform appropriate treatments and the intensity of monitoring and patient education.
- Importantly, more severe CKD (low GFR and/or high albuminuria) equals to higher cardiovascular risk.
Alternatively, you may also use following methods to determine the probability of kidney failure.
- Renal function trajectory pattern.
- Kidney Failure Risk Equation - May be useful for patient and provider communication, triage and management of nephrology referrals and timing of dialysis access placement and living related kidney transplant.
- More advanced tools, such as KidneyIntelX - Often more costly
Symptoms of CKD
At early stages of CKD, patients are largely asymptomatic.
In stages 3-5 CKD, patients may begin to experience general symptoms related to fatigue, oedema, and decreased urine output.
- Cardiovascular symptoms may arise related to hypertension, heart failure, pericarditis, and atherosclerosis.
- With the accumulation of uremic toxins, individuals may experience nausea and vomiting, anorexia, bleeding, and pruritus.
- Neuromuscular symptoms include restless leg syndrome, muscle cramps, impaired cognition, and peripheral neuropathy.
- Anaemia may also be present at the later stages of CKD due to the kidney’s inability to produce erythropoietin.
- An imbalance of calcium and phosphate homeostasis and vitamin D metabolism may contribute to signs and symptoms related to renal bone disease such as bone pain and increased risk of fractures.
General Management in Retarding CKD Progression
Nephrology referral is especially indicated when there is a rapid decline in kidney function, an elevated albumin-to-creatinine ratio (>300 mg/g) or urinary red blood cell casts.
- Treating the underlying cause, such as diabetic kidney disease, viral infections, cardiac or hepatic disorders, administration of nephrotoxic drugs.
- Reduction in proteinuria, optimization of blood pressure and blood glucose is integral in slowing the rate of CKD progression.
- Patients with proteinuria should be treated with an ACE inhibitor or angiotensin receptor blocker (ARB) and sodium-glucose cotransporter 2 (SGLT2) inhibitors.
- Nonsteroidal mineralocorticoid receptor antagonists (e.g. finerenone) are most appropriate for adults with type 2 diabetes who are at high risk of CKD progression and cardiovascular events, as demonstrated by persistent albuminuria, despite other standard-of-care therapies. To mitigate risk of hyperkalaemia, select people with consistently normal serum potassium concentration and monitor serum potassium regularly after initiation.
- Treatment with SGLT-2 inhibitors and glucagon-like peptide 1 (GLP-1) receptor agonists may reduce the risk of kidney disease progression in patients with type 2 diabetes.
- Treatment of chronic metabolic acidosis with supplemental bicarbonate may slow the rate of kidney function loss.
- Requires careful monitoring of volume status because bicarbonate is administered with sodium.
- Lifestyle modifications are encouraged in patients with CKD, such as
- To avoid sedentary behaviour.
- Undertake moderate-intensity physical activity for a cumulative duration of at least 150 minutes per week, or to a level compatible with their cardiovascular and physical tolerance.
- Maintaining optimal weight
- Avoidance of smoking
- Dietary intervention particularly protein, phosphate and sodium restriction are essential in retarding progression of kidney disease.
- Adopting healthy and diverse diets with a higher consumption of plant-based foods compared to animal-based foods and a lower consumption of ultraprocessed foods (e.g. sugar-sweetened beverages, fast foods, frozen meals, chips, candy and pastries).
- Sodium intake to be <2 g of sodium per day (or <90 mmol of sodium per day or <5 g of sodium chloride per day) in people with CKD.
A restricted protein diet with or without supplemental ketoanalogues has been shown to retard the progression of chronic kidney disease (CKD).
- However, a low protein diet [0.55-0.6 g/kg/day (0.6-0.8 g/kg/day for diabetics)] or very low protein diet (0.28-0.43 g/kg/day) plus ketoanalogues should not be started during a catabolic state in patients with CKD and should be implemented only in metabolically stable patients without intercurrent illnesses.
- A very low protein diet should be supplemented with essential amino acids and ketoacids to prevent malnutrition and power-energy wasting.
- Also, a higher dietary protein intake (1.0-1.2 g/kg/day) is recommended for patients on dialysis to maintain a stable nutrition status.
When eGFR falls below 30 ml/min/1.73 m2, nephrology referral is initiated to discuss and potentially plan for kidney replacement therapy.
Renal Webinar 2022 - Community CKD Checkpoint
External Links
- Longitudinal progression trajectory of GFR among patients with CKD, 2012
- KDIGO CPG for the Evaluation and Management of CKD, 2013
- KDIGO CPG for the Evaluation and Management of CKD, 2024
- KDOQI Clinical Practice Guideline for Nutrition in CKD, 2020
- Healthy Dietary Patterns and Incidence of CKD, 2019
- KDIGO CPG for Diabetes Management in CKD, 2020
- KDIGO CPG on the Management of BP in CKD, 2021
- Chronic kidney disease as cardiovascular risk factor in routine clinical practice, 2022
- CKD Diet: How much protein is the right amount?




Comments
Post a Comment