Dry Eye
Introduction
Dry eye (keratoconjunctivitis sicca) is a common problem, particularly in elderly.
- It causes varying degrees of discomfort.
Pathophysiology
The tear film is needed to maintain a healthy eye surface and for enabling clear vision. Tears are made up of a complex mixture of water, salts, lipids, proteins and mucus.
- The lipids, or oily component, surround the tear film and help to prevent evaporation of the water.
- The mucous component helps spread the tear film evenly over the surface of the eye.
- Aqueous deficient DED
- Decreased tear production due to Sjogren's syndrome, older age and diabetes mellitus.
- Evaporative DED
- Increased evaporative loss from the ocular surface due to meibomian gland dysfunction, structural abnormalities of eyelid position, decreased blink function, topical medicated or preserved eye drop use, chronic contact lens wear and ocular allergy syndrome.
However, it is now believed that both mechanisms are present in most patients, although one may be predominant.
NOTE: Tear production diminishes with age and is affected by female hormones, so the problem is most common in older women.
Clinical Features
Both eyes are usually affected.
Symptoms reported are eyes that burn, feel tired, itchy, irritated or gritty, with symptoms worsening throughout the day.
- The conjunctiva is not red unless irritated (e.g. eye rubbing or allergy).
Typically, symptoms fluctuate in intensity.
- Exacerbating causes include medications, windy conditions, cold weather, low-humidity environment, extend time spent looking at screens, and time of day.
Important Questions to Ask
Environment
- Windy, dry climates increase tear evaporation.
- Long periods of time spent working at a computer screen are associated with dry eye because blinking tends to be less frequent.
Medical conditions
- Patients with rheumatoid arthritis, diabetes or thyroid problems are more likely to experience dry eyes.
- Also, it is common to develop dry eye after eye surgery such as cataract or refractive surgery.
Medications
- Antihistamines, beta-blockers, chemotherapy, diuretics, HRT, oral contraceptives, SSRIs and TCAs may affect the quantity and composition of tears.
Symptoms
- Patients with dry eyes may report irritated, gritty, scratchy or burning eyes, a feeling of something in their eyes, excess watering and blurred vision.
- Initial referral to an ophthalmologist if the diagnosis is in question or if the patient has severe pain or associated visual loss, or abnormal blinking or inability to close their eyes completely.
Contact lenses
- Individuals who wear contact lenses are more likely to experience dry eyes.
Over-the-counter Medication: Treatment of Tear Insufficiency
Apart from lifestyle and environmental treatment (e.g. frequent blinking during computer use, minimize exposure to air conditioning and stop cigarette smoking or avoid exposure to second-hand smoke), dry eyes are managed by the instillation of artificial tears and lubricating ointments.
- For people with mild or moderate symptoms, artificial tears alone are usually sufficient.
- For people with severe symptoms, consider adding an ocular ointment to use at night.
Evidence of superior efficacy among any of the ophthalmic lubricants is lacking.
- Choice is based on patient acceptability and adherence as well as sensitivity/allergy to preservatives contained in the product.
- Thicker agents last longer which may reduce the number of applications needed, but may have more of a tendency to blur vision.
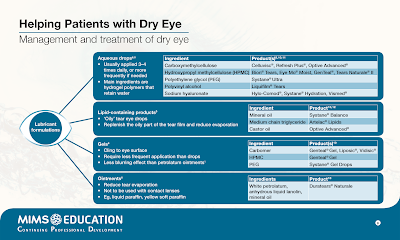
- For initial treatment, select an artificial tear containing any of 3 main ingredients:
- Carboxy methylcellulose (CMC)
- Hydroxypropyl methylcellulose (HPMC)
- Hyaluronic acid
- If symptoms are still inadequately treated, consider gel or lipid formulations, ointments, liposomal sprays, or a dissolvable hydroxypropyl cellulose insert (Lacrisert).
- For patients with refractory symptoms, try an artificial tear containing either Polyethylene glycol (PEG) or Polyglycol and glycerine.
- You may refer to this post on method of administration of ophthalmic preparations and storage.
The dosage of all products marketed for dry eye is largely dependent on the patient's need for lubrication, and is therefore given on an as-needed basis.
May consider using a preservative free product
- if a product causes irritation,
- if tear substitutes are used frequently (such as >4 times per day) and chronically
- if soft contact lenses are worn
NOTE: For patients with moderate-to-severe dry eye and ocular inflammation, ophthalmologists may consider anti-inflammatory therapies in addition to aqueous enhancement therapies, such as cyclosporine 0.05%, lifitegrast ophthalmic solution 5%, and topical corticosteroids at low-doses and infrequent intervals for several weeks.
Management of Eyelid Abnormalities
Correct any eyelid abnormalities resulting from blepharitis, trichiasis, or lid malposition (for example, lagophthalmos, entropion/ectropion) that may contribute to dry eye.
- Ensure that lid hygiene is part of the treatment regimen for blepharitis or meibomian gland dysfunction.
- Blepharitis is a common eye disorder characterized by a chronic inflammatory process primarily involving the skin, lashes, and meibomian glands of the eyelid.
- Common symptoms in patients with blepharitis include sore eye lids, irritated eyes, gritty eyes, dry or water eyes, increased frequency of blinking, foreign body sensation and eyelids sticking together (especially in the morning) (i.e. crusts at the lid margins).
- Consider treating inadequate lid closure with nighttime eyeshields which mechanically close eyelids or forced temporary closure of lids by patching or taping.
- Incomplete blinking or an inability to close the eyes fully during sleep can result in drying of the ocular surface.
- Consider surgical correction of other eyelid abnormalities, such as entropion and ectropion, conjunctivochalasis, dermatochalasis, and severe conjunctival disease.
- Entropion (eyelid turning inward) and ectropion (eyelid turning outward) result in increased ocular surface exposure, causing symptoms of dry eye.
- Conjunctivochalasis is loose, redundant, nonedematous inferior bulbar conjunctiva located between the globe and eyelid. It is an age-related ocular disorder that is often overlooked.
- Dermatochalasis is a common condition with skin redundancy and lid atrophy of the upper eyelids mostly caused by aging.
Eye lid hygiene
- Apply a warm compresses to eyelids for several minutes to soften adherent scurf and scale or to discharge and/or warm meibomian secretions.
- Compresses and massaging eyelid 1-2 times/day at a time most convenient for the patient is generally sufficient.
- Adherence is often poor due to the time required and difficulty in maintaining the temperature of the compress for extended application.
- Crusts can be removed using any of the following:
- Cotton balls
- Cotton-tip applicators
- Commercial eyelid scrub or 50:50 mix of water and baby shampoo on a quilted makeup remover pad
- Hypoallergenic soap
- Sodium bicarbonate in water
NOTE: In blepharitis patients with symptoms refractory to lid hygiene, consider topical ophthalmic antibiotics ointments and/or short-term topical ophthalmic corticosteroids.
Supplements
Increasing systemic omega-3 essential fatty acid levels through nutritional intervention has been suggested to provide systemic anti-inflammatory effects that aid in the production of tears.
- American Academy of Ophthalmology (AAO) suggests that oral fatty acid supplements may not be effective for patients with moderate to severe dry eye, but they may be helpful as adjunctive therapy in patients with blepharitis.
- Omega fatty acids are contraindicated in patients with liver disease, atrial fibrillation, or bleeding disorders.
External Links
- Over the counter (OTC) artificial tear drops for dry eye syndrome, 2016
- TFOS DEWS II Definition and Classification Report, 2017
- Master the Maze of Artificial Tears, 2018
- Artificial Tears: What Matters and Why, 2020
- Omega-3 fatty acids in the management of dry eye disease-An updated systematic review and meta-analysis, 2022
- AAO - Can Fish Oil Relieve Dry Eye?, 2024
- AAO - What Is Blepharitis?, 2023




Comments
Post a Comment